A Journey From Caregiver to Student, Ostomy Patient, and Nurse
My name is Jennifer Borchek, and I am a recent graduate of Chamberlain University with a Bachelor of Science in Nursing. I am a licensed registered nurse. I also have a colostomy. While I know that my condition changed a part of me, I also know that it has never defined me, my career choice, or who I have become.
A Career Path of Care
My passion for nursing stems from the love and care that I showed for my ailing grandmother during her time of need. My grandmother suffered from many health issues that demanded around the clock care. At the age of 15, my mother and I became the primary caregivers for my grandmother, so we relocated into our grandmother’s home to care for her as her needs increased. This responsibility was not something I took lightly. I spent many nights rushing down the stairs to my grandmother’s bedside when I would hear the slightest sound that might mean she needed attention. Eventually, the running up and down the stairs and the weight of my worry became too much; I picked an empty spot on the floor near my grandmother where I would sleep with one eye and ear open. By the time I graduated high school, I had developed a good sense of care and a strong interest in continuing my path in health care. I decided what better way to use my experience than to become a certified nursing assistant?
After my certification, I attended a local community college to complete my general education requirements and earn an Associate Degree of Science with honors. This brought me closer to my dream career of becoming a nurse. During this time, my grandmother passed away, and I took a break from school to work in a nursing home. My caring nature was fulfilled at my job by helping others know that their loved ones were well attended to. While working in this environment, I knew I could achieve more, and I decided to apply to nursing school to begin my path as a registered nurse. Soon after, I was accepted into a Bachelor program for nursing. I knew that it would be a challenge to continue my education, as balancing school, work, and family could be difficult, but I also knew that my dream and ambitions were strong. I was ready to face the academic and scheduling challenges ahead, but I was not prepared for the unexpected health issues that I encountered along the way.
A New Path with a Slight Turn
One day, while walking between classes, I started to feel a nagging pressure in my genital area. It became sporadic and seemed to have no pattern or reason for occurring. It would oddly come and go regardless of what I was doing at the time. I thought it would just go away, but it persisted. I spent countless months going back and forth to the gynecologist with the same concern. Consistent medical testing provided no reasons for the pain. For more than a year, I felt as though I was wanting and eventually begging to be heard by the doctor. Examination after examination, I started to think that maybe this was all in my head, and at times some doctors and nurses suggested that too. This was eventually disproved one evening when I felt a sudden burst of blood run down my legs after a hot bath. I rushed to the emergency room only to be told that I was “fine” and to follow up with my gynecologist. I went home that night heartbroken and confused; how could this not be enough to diagnose my health issue? So, yet again, I booked another appointment and headed over to the gynecologist’s office that I’d been to so many times before. After I was examined, the doctor removed her gloves, looked at me and said, “This is not your vagina anymore; this is your rectum. Go to the colorectal surgeon and tell them that you’re bleeding.” She walked out of the room without saying another word. I couldn’t even begin to comprehend what she was saying. Why would I need a surgeon? What does a colorectal surgeon have to do with my vagina? I was filled with a furious, confused, frustrated rage, and I was scared. I left with more questions than I arrived with, and now I was heading into unfamiliar territory. Did I have cancer? What kind of surgery would I need?
I later booked an appointment with a knowledgeable and focused colorectal surgeon at a well-respected teaching hospital. It took three very long weeks for my appointment date to arrive.
Diagnosis over Despair
I met the colorectal surgeon and he told me I had to be diagnosed under anesthesia. He suggested it was an anal fistula during the initial appointment. I was not sure what this diagnosis meant or how it happened, but in all, I liked and trusted this doctor. I felt as though I finally found someone who understood what I was going through and could diagnose what I had been complaining about for over a year. I scheduled the procedure during my one-week break from school. I liked that the doctor not only respected me and my concerns and feelings, but I also appreciated that he was very understanding of my desire to become a nurse. He helped me understand that my condition would not prevent me from living a normal life and achieving my degree.
Weeks later, I underwent anesthesia to be diagnosed. My surgeon told me after that I needed more surgeries to treat my newly discovered health issue. I had a rectovaginal fistula and he informed me that I had had it for at least five years. He also stated there was no exact reason why I had developed a fistula. While this made complete sense looking back at all my symptoms, I still cried when I heard this report. Suddenly, all the missing pieces were finally fitting together.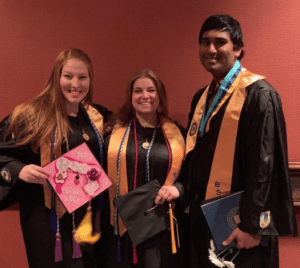
I had a diagnosis, but this was not the end of my battle. I underwent six separate surgeries all while maintaining honors in nursing school. The most recent was my ostomy surgery. During this time, I dropped down to only taking one class and had been unable to work a career-related job because of my health needs. The hours of studying were long and strenuous, but I fought through recovery one day at a time. Hauling heavy books and running from class to class were no longer a part of my day. Healing was just as important as learning, and I managed to balance the two. I often studied while soaking in the bathtub, as this was the doctor’s order to help the healing process.
During the increased workload of nursing school, I met two very caring friends, Laura and Bert, who helped me along the way. They were there for me when things got rough and made sure I didn’t fall behind in school during my health obstacles. I asked for health-related accommodations and was able to have Laura and Bert with me in every class and during clinical. This was a way to be sure that I would have the support and care if necessary. As a new ostomate, I knew anything can happen spontaneously. Having caring and trusting friends nearby encouraged me to relax about my condition and focus on my studies.
More Frustration, but Still Focused
Throughout my path, I was somewhat saddened to learn that ostomy surgery was a necessity. I understood that my fistula was not healing with the multiple surgeries that were performed, so the ostomy became a part of something I learned to accept. Even now my focus is to heal, rather than stress the need to reverse my ostomy before my fistula has completely healed. I was informed by my colorectal surgeon that rushing the process could result in the same challenges I had when I started my journey.

Jennifer with her close friend Jenell, left, whom she met at a UOAA Affiliated Support Group Meeting in Illinois.
Finding Friendship and Support through the Flaws
During my hospital stay for my ostomy surgery, my Wound, Ostomy and Continence (WOC) Nurse informed me that the Loyola University Medical Center held monthly ostomy support group meetings (One of 315 UOAA Affiliated Support Groups in the U.S.) and that she thought it would be beneficial for me to attend. She mentioned a young woman around my age who had recently had surgery. I thought it couldn’t hurt to show up.
I hoped to gain tips on care, products and living life differently with what seemed to be a flawed digestive system. I had already researched some of this online and in magazines, but I decided that more information could not hurt. Three weeks after major surgery, I walked through the door of the meeting room, still in pain and feeling a bit awkward about the whole thing. I sat down behind the youngest person in the room. She turned around and immediately greeted me with a friendly smile and introduced herself and her mom to me. She is in her late 20’s, her name is Jenell, and her stoma’s name is Piglet. Suddenly, I didn’t feel so nervous when Jenell asked why I came to the meeting. When I told her my story she said that it was unlike any story she had heard before. We spent the rest of the meeting talking about all things ostomy. We exchanged telephone numbers after the meeting and quickly became good friends.
Jenell eventually shared her own story with me and the story of naming her ostomy. Most ostomates feel naming their stoma helps them accept the transition of having an ostomy. With Jenell’s encouragement, I named my stoma “Rosita,” symbolizing that an ostomy reminds me of a rose. Jenell has helped me in so many ways by encouraging me about my health condition; she gave me confidence and showed me that even though my body changed, it doesn’t mean I changed as a person. She also taught me how to handle certain situations. For example, because of our invisible illnesses, we feel the need to educate the public on unseen chronic physical conditions. Together, the four of us – myself and Jenell and our stomas, Piglet and Rosita – make quite a team. We have a lot to be concerned about, but we also have a great future and much to be thankful for. We’ll face more challenges, but we’ll do it together.
My own experiences have helped me decide that I want to become a WOC Nurse and tell others with the same condition that they also can live a normal life. I want to help others with the transition of becoming an ostomate. I want others to know that they can follow their dreams, share their successes, lead by example, and show care from their experiences. I decorated my graduation cap to celebrate my decision and I included Rosita in my design to recognize that I have successfully overcome my challenges, and to show my ostomy is part of me and part of my future.
I am ecstatic to be sending out applications to be hired as a registered nurse because I never thought this day would come due to all my uncertain health issues. However, I will have to wait until my next surgery and through recovery. I know I’ll get there eventually because my challenges will not stop my dream!
Appreciation
All in all, I am very grateful for those I have in my life who have supported me: for Jenell for her friendship, for my surgeon with his knowledge and talents, for the WOC nurse that helped me get through my transition of being an ostomate, for my instructors for teaching me so well, for my classmates Laura and Bert and all the support they gave me, for Rosita for being so accommodating of my ongoing issues, and most importantly for my mother to whom I attribute my success. She encouraged my caring nature, has kept me strong and motivated, has lifted me when my spirits were low, and she is the reason I have fought so hard to become a registered nurse!