Expect More – Take Control of Your Health Care
Part 1 in Series
By UOAA Advocacy Committee
This first article is about finding your voice as you take the initiative to speak up, or act on your own behalf, to encourage change that will bring improvements in your quality of ostomy care, and ultimately, your quality of life.
We are all unique individuals and regardless of having a medical condition such as an ostomy some people by nature are outgoing while others are more naturally shy and timid. Some people are overly confident while others lack self-esteem. We are who we are; however, when it comes to your health and well-being, if your gut is telling you “this isn’t normal” or something is wrong or you just don’t plain “get it”, don’t be afraid to speak up. There is power in your words. Yes, this can be easier said than done for many, but realize there is no shame in asking for help. It can be a challenge to balance being assertive while not being overly demanding.
Ask yourself the question – do you think you are capable of producing a change? How do you create change in your life? For example, if you are experiencing pain and sores on the skin around your stoma – are you accepting this as normal and trying the best you can to manage it on your own because you don’t want to bother anyone? In contrast, are you someone that would call your doctor, seek resources to find help and not accept this as normal? It is good to try to be self-sufficient but if you are still suffering and in pain then a positive change has not happened. What can you do to strengthen your voice, and be a participant in your self care? The belief that you can make a change is called self-efficacy. It is a little different than being self-confident in that you truly believe a change will happen and you won’t stop seeking help until that change has happened.
Some people also fear that by speaking up and questioning their healthcare providers, that they will find them annoying, stupid, needy or unlikeable. Healthcare professionals are held to high medical standards and they want to help their patients. They understand that this is new to you and that you are trying to understand your medical condition. They also need you to understand your treatment plan, so that it can be a success. There is absolutely no reason to feel embarrassed. Remember, if you do not ask your questions or express your concerns, you remain uninformed and that is a fearful place to be. You want things to get better not stay the same.
FIND YOUR VOICE: 10 Questions To Ask Yourself
When it comes to medical situations, many people become tongue-tied or have difficulty expressing themselves. UOAA recognizes that it is not enough to just tell ostomates to self-advocate, but rather we need to provide you with the tools to do so. Self-advocating can be a positive experience.
Below are 10 questions and simple solutions that will help you find your voice:
1) Are you nervous, anxious or confused about your medical condition?
People who do not feel confident in their understanding of their medical condition feel fearful. Once they are educated about their condition, they are more confident to speak up. The information in this blog post and UOAA’s ostomy information and educational resources can help you gain confidence and if you are just starting your ostomy journey it can give you a sense of control in a time of uncertainty. “Knowledge is power.” ~ Sir Francis Bacon
2) Do you just defer to the expertise of medical professionals or do you participate in decision making?
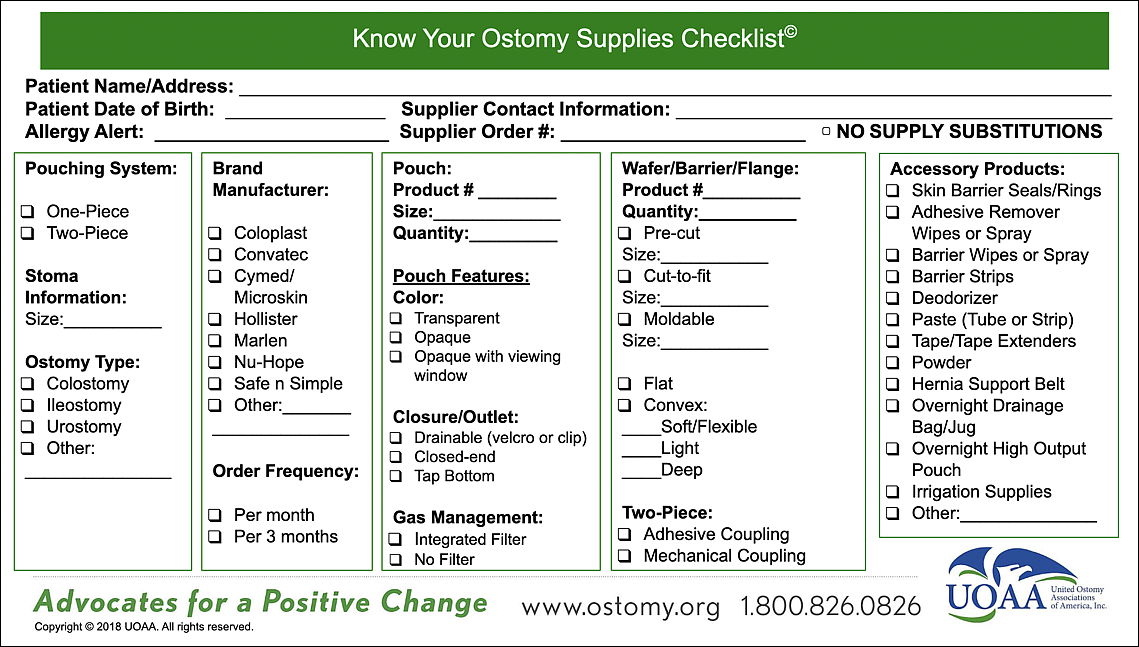
Many people assume they have no role in their care. They just leave it in the professionals’ hands. In reality, you play a very important role. Medical “lingo” is very new to people – people who don’t understand it do not feel confident in speaking up and feel intimidated by medical professionals. Most people are afraid to say – I don’t understand what you are saying. Make a list of what you do and don’t understand to generate the proper questions to ask.
3) Do you think you are the only one in the world having these issues and concerns?
People who feel alone do not speak up – once they find others such as with a support group – they feel more confident and less isolated and alone. Here you can get a role model or peer to guide you along the way. It’s comforting and insightful to hear from people who share similar experiences. Chinese proverb: “To know the road ahead, ask those coming back.”
4) Do you have low self-esteem and sometimes feel that your life doesn’t matter?
People with low self-esteem tend to not speak up. They tend to remain silent or let other people do the speaking for them. When someone has low self-esteem, it is hard to see his/her own worth or recognize that his/her opinion matters. Self-esteem is further affected by a life-altering/body altering illness such as ostomy surgery. Take steps to feel better about yourself or if needed, seek counseling.
5) How can advocating for your healthcare needs (or other things in your life) really change your life in a positive way?
Consider the impact on your life. Make a list of pros and cons for speaking up. If the pros outweigh the cons, it may be worth it to speak up and improve your life in a positive way.
6) Do you have a concern or health issue with your ostomy, but your doctor or nurse pushes it aside and tells you not to worry about it?
Are you the type of person if you are worried about something, but your doctor doesn’t mention it, then you assume it must not be a concern so you remain silent? If you are unsure or disagree and it is affecting your quality of life, then get a second opinion by another expert. Listen to your gut. It’s important for you to feel safe and secure in your own body, and you certainly don’t want the problem to get worse (or it might truly be nothing to worry about!). It always feels better to have your concerns addressed in a way that makes you feel that you have been heard.
7) Do you find yourself rushed or brushed off when you are at an appointment with a medical provider?
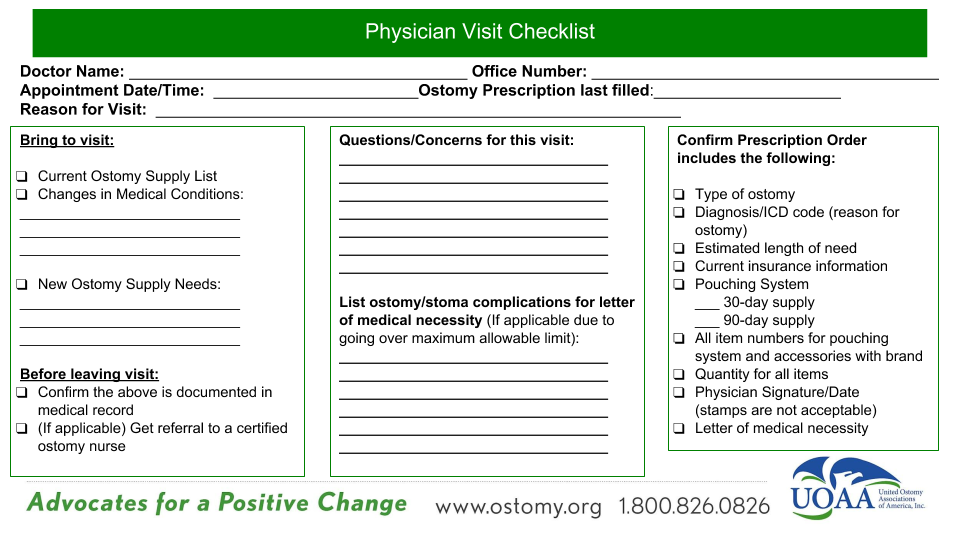
We all agree that medical professionals are busy and are often running behind schedule. The good news is that often this occurs because other patients were asking questions during their appointment! They were speaking up! You deserve their time too. Write down your questions before you arrive and be sure to take out your list and go over every single question you have. Remind yourself – this is your visit, this is about YOU, not the doctor. Also, the next time you call to make your appointment tell the office staff that you will need some extra time to discuss all of your concerns and evaluate your situation especially if it is a complicated issue.
8) Do you feel like you are just another ostomy patient in a long assembly line and feel that there is no real care for YOU, a unique and individual person?
If you consistently leave the office feeling worse than when you entered and with unanswered questions, then it is time to consider finding a new provider and seeing someone else who will make you feel comfortable to ask questions and take the time to listen and respond. This holds true even if it’s a referred provider who is supposedly the “best” in the field. It’s important to have a good relationship with your provider. Quality ostomy healthcare is a team effort and communication is critical.
9) Have you ever looked back and kicked yourself for not saying something?
It’s better to speak up, than have regrets later, especially when it might be something as serious as your health and well-being. Your doctor has many other patients and concerns on his/her plate so don’t run the risk that they will remember everything about you or what was discussed at your last visit together. You know your health history. You are the person experiencing the symptoms or whatever the issue is. It is absolutely your place to express your concerns.
10) Do you sometimes draw a blank or choke under pressure and miss out on speaking up?
Keep an ongoing list of your questions and concerns prior to meeting with your medical professional. Practice the conversation that you want to have by role-playing with a family member or friend acting as your doctor or nurse. Practicing will help instill confidence in what you want to say. You can also decrease stress by bringing your questions with you and reading them from your paper. That way you are sure that nothing is forgotten. “Asking for what you need, what you want, and what you’re worth requires practice. So practice self-love and start asking.” ~ AnneMarie Houghtailing
FIND YOUR VOICE: Expect More Examples of when you or your Advocate should speak up!
IF YOU CAN’T FIND YOUR VOICE; BE SURE TO GET AN ADVOCATE
We realize that having major surgery can be overwhelming. Be sure to find someone who can help you along the way. Sometimes you might “lose your voice” especially after surgery, from medications, or just being overwhelmed. Your advocate should be someone close to you, whom you can share your deepest fears and concerns with, and HAS A VOICE, and can speak up for you when you can’t. Your advocate can ask questions for you or simply listen and take detailed notes so you can recall and understand later.
SPEAK UP!
If English is not your primary language, you have a right to an interpreter. All hospitals are now required to have interpreter services either in-person or via web connections provided for you.
In conclusion, we know that ostomy healthcare is not perfect and inconsistent in our country. When it comes to your healthcare, don’t be shy. You must harness the power of your own voice and share your concerns, desires, and opinions; because if you don’t, who will? Remember that you matter! You are important! Self-advocacy isn’t a “one and done” deal. It’s an ongoing process from before you have your surgery thru the ongoing continuum of care of your ostomy or continent diversion.
Speak Up! Ostomy and Continent Diversion Patient Advocacy Resources:
(Note – Although we focus on finding your voice with regards to healthcare, you can use these self-advocacy tips in other areas of your life as well.)






 After eight years of not responding to western pharmaceuticals, at the age of thirty, I found myself facing a colectomy. While I had anxiety about the ostomy surgery and fear of the unknown, my overall emotion was relief. This surgery was hopefully going to be the end of many years of pain and suffering. Thanks to the encouraging words of other ostomates I was wheeled into surgery with a smile on my face, excited about what the future would hold for me–I saw endless possibility!
After eight years of not responding to western pharmaceuticals, at the age of thirty, I found myself facing a colectomy. While I had anxiety about the ostomy surgery and fear of the unknown, my overall emotion was relief. This surgery was hopefully going to be the end of many years of pain and suffering. Thanks to the encouraging words of other ostomates I was wheeled into surgery with a smile on my face, excited about what the future would hold for me–I saw endless possibility!


