Thanks to the ongoing generosity of the ostomy community donating to UOAA’s scholarship fund, we were able to provide this award in the amount of $3000 to another nurse. UOAA is excited to announce that the 2023 recipient of the Educational Award for Ostomy Nurse Certification is Ashlee Cranage from California!
Below a grateful and honored Ashlee shares a little bit about herself and her motivation to become a certified ostomy nurse.
My name is Ashlee Cranage and I am so honored to be the recipient of UOAA’s Educational Award for Ostomy Nurse Certification. Becoming a certified ostomy care nurse is no easy task, and I am grateful to be recognized by UOAA as I strive to make a difference in the ostomy community.
I joined Community Memorial Healthcare in Ventura, CA as a new graduate registered nurse six years ago, starting out on the post-surgical unit. In March 2022, I joined the inpatient Wound and Ostomy Care Department working alongside both a certified Wound Ostomy Continence (WOC) nurse and a certified wound specialist (CWS). This job opportunity has opened my eyes to the impact that certified ostomy nurses bring to the healthcare field, and most importantly patient care. I became a Certified Wound Care Nurse (CWCN) in September 2022 and became a Certified Ostomy Care Nurse (COCN) in April 2023.
One thing that I have learned this past year is that there is such a need for certified ostomy care nurses, and I am excited to be able to contribute to that need and make a difference!
Prior to working in wound and ostomy care, my ostomy knowledge and skillset was very limited. I could proficiently change a simple pouching system, but I did not have the confidence to troubleshoot a leaking pouching system, nonetheless teach patients adequately about their ostomy care post-surgery. Once I began my new role, I started seeing patients with ostomies more frequently and I knew I needed to be more comfortable with their ostomy care. Following our certified WOC nurse periodically and being present for the meaningful conversations and positive impact that she had on her patients, made me want to further pursue my education to do this too. Being present for those hard conversations, watching her connect with her patients and continue to follow up with them post discharge as well, motivated me to be able to also achieve this higher skill level and knowledge to make an impact.
With my recent certification in ostomy nursing, I now have the knowledge to better my nursing practice and care for the patients with ostomies that our department sees on a day-to-day basis. I have the expertise to be able to be there pre and post-surgery, help patients navigate life with an ostomy and support them throughout their journey. I aspire to continue to work alongside my colleagues with the creation of a free ostomy clinic for our community to better be able to help and support at any time during their ostomy journey, whether they’ve had it for 2 weeks or 20+ years. I also aspire to be a support system for my patients by joining my colleague in holding a monthly ostomy support group where individuals can come together to share their experiences, tips and tricks and seek information or support that they may need. For some, getting an ostomy, whether it is elective or emergent, may be a scary situation in the beginning. However, having a certified ostomy care nurse to help navigate any challenges and provide information and support can turn a scary situation into a learning opportunity full of hope and willingness to learn.
One thing that I have learned this past year is that there is such a need for certified ostomy care nurses, and I am excited to be able to contribute to that need and make a difference!
Congratulations, Ashlee!
The next scholarship application will open, pending funding availability, in January 2024 and closes on June 30, 2024.
If you’d like to donate to the Ostomy Nurse Scholarship Fund online, please complete the Donate Form, and at the bottom under the ”Additional Comments” section, please note “Ostomy Nurse Scholarship Fund”. You can also send a check made payable to UOAA, in the memo line include the Fund name, and mail to PO Box 2293, Biddeford, ME 04005-2293.







 the next few years they met up in New Orleans, Virginia, Cleveland, Hartford and of course at the next UOA conference in 2005 in Anaheim.
the next few years they met up in New Orleans, Virginia, Cleveland, Hartford and of course at the next UOA conference in 2005 in Anaheim.

 For me, I plan to get back to my full fitness routine once I am fully recovered. I already feel healthier than I have for so many years. But I know I still have a lot of learning to do… from
For me, I plan to get back to my full fitness routine once I am fully recovered. I already feel healthier than I have for so many years. But I know I still have a lot of learning to do… from 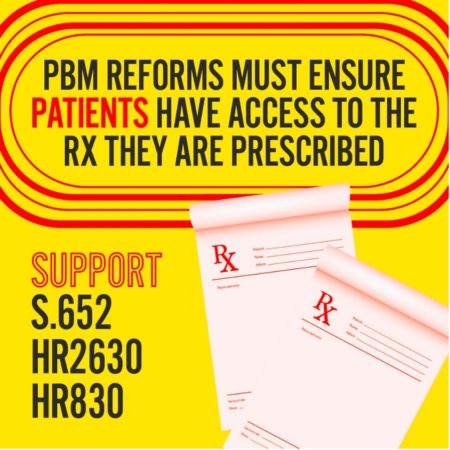 (DDNC) and the Safe Step Act Coalition where we share common goals and work together to achieve them. For example, the DDNC’s mission is to work cooperatively to improve access to and the quality of digestive disease health care in order to promote the best possible medical outcome and quality of life for current and future patients. Although UOAA is unable to have its own “ostomy” lobby days or fly-ins on the Hill (due to financial limitations), we are an important part of the annual DDNC Spring Public Policy forum. Ostomy advocates join forces with other digestive disease advocates to meet with Congressional staffers to share their stories and ask for support of our federal legislative priorities. These coalitions submit joint letters of requests or support/opposition to Congressional leaders and key regulatory decision-makers. An example of power and strength in numbers is the Safe Step Act Coalition which now comprises 215 patient organizations all advocating for passage of this important piece of legislation!
(DDNC) and the Safe Step Act Coalition where we share common goals and work together to achieve them. For example, the DDNC’s mission is to work cooperatively to improve access to and the quality of digestive disease health care in order to promote the best possible medical outcome and quality of life for current and future patients. Although UOAA is unable to have its own “ostomy” lobby days or fly-ins on the Hill (due to financial limitations), we are an important part of the annual DDNC Spring Public Policy forum. Ostomy advocates join forces with other digestive disease advocates to meet with Congressional staffers to share their stories and ask for support of our federal legislative priorities. These coalitions submit joint letters of requests or support/opposition to Congressional leaders and key regulatory decision-makers. An example of power and strength in numbers is the Safe Step Act Coalition which now comprises 215 patient organizations all advocating for passage of this important piece of legislation!



