Ostomy Day or Ostomy 5k- This is the Time to Get Involved
Whether you attend an in person or virtual event, make this be the year you get off the sidelines and discover the power of ostomy awareness. Learn more about all the ways to get involved on our Ostomy Awareness Day (OAD) web page.
“Ostomies Are Lifesavers” – this simple message can pack a big punch when you hear it from someone you know. Whether you post to friends and family on social media or confide in a few people, it can help dismantle stigmas and open hearts and minds. Everyone benefits when you state “I Am Living Proof that Ostomies Are Lifesavers” and reflect on the life you have enjoyed because this surgery exists.
To share your message with UOAA and others consider sharing a video, photo or statement on our online Wall of Love. #IAmLivingProof #OstomiesAreLifesavers
Virtual events to celebrate OAD
Events this week kick-off on Thursday, October 3, with a special Virtual Art Expression Class in collaboration with Connecting Pieces. Have fun, experience some artful healing and connect with others to decorate an ostomy pouch or anything you’d like. Register today! $10 child, $25 Individual, $35 Group
On Saturday, October 5, Ostomy Awareness Day, WOCN® Society is hosting a virtual Ostomy Education Day. Caregivers, medical professionals seeking CRE credits, and anyone in the public wanting to learn more about ostomy care are welcome to join this free event.
On Saturday you’ll also have the chance to connect directly with our inspiring Ostomy Awareness Day Champion Kimberly Holiday Coleman. Visit UOAA’s Instagram Page @UOAA_ at 12 noon Eastern Time (9am Pacific Time) for a special Instagram Live Q&A – and feel free to ask her anything!
The Ostomy 5k- Not just for Runners
It’s a celebration of resilience and a gathering of ostomy awareness supporters no matter how far you can walk, run or roll. Virtual 5k participants have gone the distance by using a treadmill, swimming, kayaking, riding stationary bicycles, and even horseback riding! Be sure to share your photos no matter where you do it!
The in-person Run for Resilience events are a mix of timed runs and fun runs as well as scenic walks and all are very family-friendly. Registration is still open and everyone is welcome to participate or simply gather and cheer on the resilience of the ostomy community!
The events are held on scenic greenway and park locations in Durham and Birmingham, city walkways outside Chicago in Downers Grove, riverside trails in Nashville and Northwest Arkansas, to mountain valleys in the Poconos of Pennsylvania and Meridian, Idaho.
The Trumbull County Ohio walk/run is ready for any weather. It will take place on an indoor track at the Niles Wellness Center. They’ll have a free mobile health screening service, a raffle and refreshments.

Locations like North Carolina are just as well known for their amazing silent auction items that are not to be missed. Local DJs, like Susie Q in Rogers, Arkansas, add to the festive atmosphere of these events.
All events have snacks and hydration and a variety of local and national sponsors’ tables to visit.
Celebrate with our Run for Resilience Sponsors
Sponsors add to the fun and awareness atmosphere of our Ostomy 5k Events Nationwide.
Coloplast is the Exclusive Diamond Sponsor of this year’s Run for Resilience Ostomy 5k. Representatives will be on hand to answer your questions and show off supplies at the events nationwide with the exception of Alabama. Check your race bags for a special sticker and magnet as well. Coloplast is also hosting an Ostomy 5k event for staff on the campus of their Minneapolis headquarters.
questions and show off supplies at the events nationwide with the exception of Alabama. Check your race bags for a special sticker and magnet as well. Coloplast is also hosting an Ostomy 5k event for staff on the campus of their Minneapolis headquarters.
Revel, a new national sponsor this year, is excited to be a part of Ostomy Awareness Day and proud to be supporting UOAA’s mission to advocate for the ostomy community. Revel will be hosting a “no-pancaking” breakfast with a full waffle bar at the founding race in Durham, NC! They’ll also be serving up samples of It’s in the Bag and free swag at booths in Durham, NC; Niles, OH and Downers Grove, IL.
Hollister is proud to be a returning sponsor this year and will have representatives and fun activities at all the national event locations. As we approach #OstomyAwarenessDay on October 5th, Hollister wants to hear about your plans to celebrate the ostomy community! For ideas on how to get involved, take a look at their activities.
Other Gatherings Nationwide
For more opportunities to meet others and learn about ostomy products check our UOAA Event Calendar for info on Ostomy Fairs and Affiliated Support Group gatherings being held to celebrate the day.
Don’t forget to let us know how you choose to make a difference on this day or in the future. Whether you got a proclamation passed where you live, or want to model that ostomy awareness t-shirt we want to see it! Email us at info@ostomy.org.


























































 “golden toilet trophy” engraved like The Stanley Cup! “It was a fun way to get people involved, a good conversation piece for anyone walking by the nursing station,” DuPree says.
“golden toilet trophy” engraved like The Stanley Cup! “It was a fun way to get people involved, a good conversation piece for anyone walking by the nursing station,” DuPree says.


 sleeping. I couldn’t stand a lot of smells or people- so not much socializing.
sleeping. I couldn’t stand a lot of smells or people- so not much socializing.  that you had to find through a scavenger hunt.
that you had to find through a scavenger hunt.
 way that is taboo or sometimes uncomfortable to discuss. In a world where it is easy to stay isolated and afraid of connection, I have found some of my closest companions were waiting for the same opportunity; hiding away behind their shields of invisibility.
way that is taboo or sometimes uncomfortable to discuss. In a world where it is easy to stay isolated and afraid of connection, I have found some of my closest companions were waiting for the same opportunity; hiding away behind their shields of invisibility.
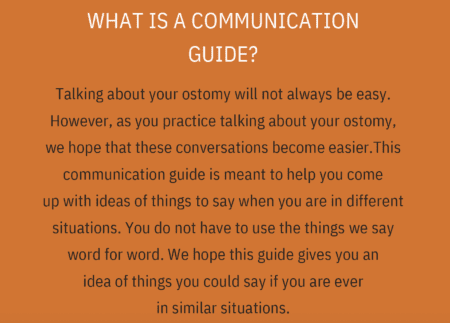 experts, and health communication experts. This guide is freely available
experts, and health communication experts. This guide is freely available 
 people to remember that no one knows that the noises came from the ostomy. It is ok to say nothing (low disclosure). It is also ok to say: “Excuse me, I have an ostomy pouch and sometimes it makes noises” (medium disclosure).
people to remember that no one knows that the noises came from the ostomy. It is ok to say nothing (low disclosure). It is also ok to say: “Excuse me, I have an ostomy pouch and sometimes it makes noises” (medium disclosure).

