By Robin Bergstein Berman
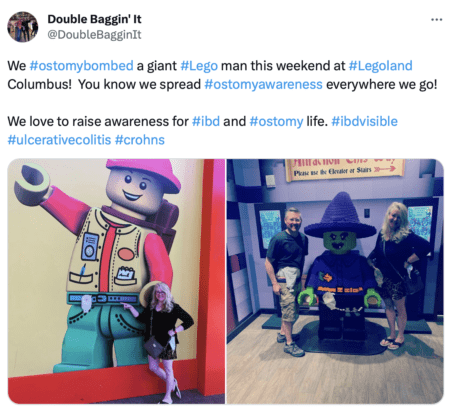
The latest episode of Larry David’s, Curb Your Enthusiasm was called “The Colostomy Bag” and during an attempt to be humorous, his usually (awkward and despicable character) made disparaging comments relating to ostomates. At least it opened up room for discussion… It’s the first time that I posted on my Facebook page about my one-and-done Ileostomy surgery 48 years ago and I received nothing but words of support. I shared below why I found the episode harmful:

“Being an ostomate does not define me.” Says Robin, 63, and has had her ileostomy for 48 years, finding health and a full life after ulcerative colitis.
This is too important not to address so I’m about to “out” myself for those who do not know. Larry David’s, Curb Your Enthusiasm episode that aired tonight was called “The Colostomy Bag” and it was harmful for a few reasons. I’m able to laugh at myself but this was not funny mostly because it passed along inaccurate information and promoted public stigmas that could cost lives. Those who desperately need a life-saving surgery (for bowel diseases, cancers and more), often put it off far too long due to inaccurate public opinion including that of too many doctors.
There were three primary comments that were said, I want to address about the episode while giving only a glimpse of my journey. First of all, not all who have an ostomy have a colostomy and therefore do not wear ”Colostomy Bags”. Larry kept saying colostomy as if it encompassed all ostomies… it doesn’t.
Secondly, having an ostomy is not the worst thing that anyone could possibly have. He made it sound as if it is. It’s life-saving and has given me personally 48 more years of life to date that I wouldn’t have had without the complete colectomy/Ileostomy I was given in a nine hour surgery in 1975. I would not be here without it since I was bleeding to death and not able to recover after given the maximum doses of steroids for an extended period of time. Polyps, the breeding grounds for cancer cells were present and multiple were seen when my entire colon and rectum were removed at 15 years old. The pain I endured prior to surgery was unfathomable and I won’t here expand on all of what I experienced. I had the most severe chronic ulcerative colitis, spending weeks and months at a time in the hospital from 11 to 15 years old.
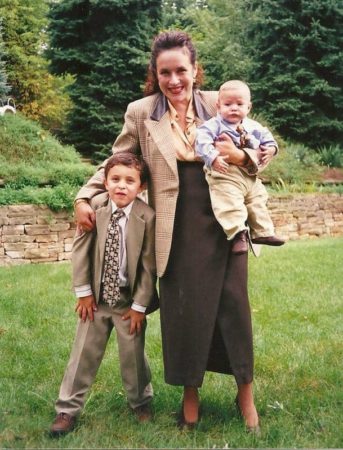
Robin with her two, now adult sons, whom she carried to term and had by emergency c-section after her ileostomy surgery.
Back to the episode; there is no such thing as a “shit in the bag look” for anyone thinking there is, like Larry. It was only slightly humorous in the context, but for someone facing this surgery and not knowing, there is no facial indications that we wear an appliance/pouch/bag. Now when he felt guilty about his comment to the car salesmen and wondered if he could gift a Louie Vitton Illeostomy Bag, that I’d like !!!…lol THIS was funny when Larry brought it up.
While they did say the car smelled like smoking, they alluded to it smelling like the man’s ostomy bag which is also not a “thing”. Popular public thinking is that ostomates smell, are unattractive, unappealing, not sexy or sexual and should be pitied. This too is not true. Within months after my surgery, I was at the beach away with my friend and her family, continued my relationship with my first boyfriend and went onto have others, didn’t miss a beat with school and countless other activities which were extensive and then went onto college away two years after my surgery. I’ve lived a full, active, useful life, carried both of our sons to term, working primarily but not exclusively in fragrance and cosmetics and certainly do not smell bad being told my entire life that I smell good (lol). In fact the first thing that attracted my husband to me was how I smelled at a bar after fragrance modeling all day.
I wear almost everything I want with some exceptions and am fashionable according to most. I’ve heard from too many that someone would rather be dead than to wear an ostomy bag. It’s the most absurd thing I’ve ever heard all caused by antiquated public opinion that is not valid and what this last episode of Larry David continues to promote.
I was going to wait until my 50-year anniversary with my ileostomy to reach out and make myself available but this prompted me to do it sooner.
Without fail when TV, even medical dramas, present ostomy surgery and the wearing of an appliance, they present it unfairly, wrong and impose additional stigmas. Don’t misinterpret me since adjusting to it sucks and there are challenges but it’s totally doable and makes a person no less the person they were in any way other than making them hopefully healthier.
If any one of you are facing this now or in the future, I am more than willing to help you or anyone you care about, to get through and adjust by listening, empathizing and giving you the tips and tricks I learned from a lifetime, 48 years, through all stages and phases of life.

Robin and her husband of 34 years.
It’s so much easier to find info today with social media than when I learned to adjust on my own without an ostomy, now a community is a click of a phone away and with laser surgery lessening the more invasive total cutting my body went through.
I was triggered tonight by the episode knowing how people are discouraged by doctors and the public’s misconceptions, I just had to address it not for me but for others. Ostomates are all ages and sexes and all walks of life including some professional athletes. Please let me know if you have any questions but mostly if you or a loved one are facing this life saving surgery, I’d be glad to help.If anyone would like to share my post, I’ll be glad to make it shareable by allowing public access. Let me know.
I was going to wait until my 50-year anniversary with my ileostomy to reach out and make myself available but this prompted me to do it sooner. I help where I can in the support groups and over 48 years ago tried forming a youth group here in Pittsburgh for ostomates, spoke to auditoriums full of high schoolers at various schools trying to discuss differences and acceptance for all and was always received well. I went on a local talk show regarding my surgery back in 1975. Being an ostomate does not define me so I spend little time discussing it unless I can be of help or it’s in a relevant conversation, which it is this week!
Editors note: The humor of the Larry character in Curb Your Enthusiasm is often built around his selfish and ignorant views. In past episodes with characters who are disabled or have a disease, those characters are usually used to help magnify his faults. This episode did not include an ostomate character just the perception of what one would be like and what life would be like with one. The opportunity for awareness, such as what Michael J Fox brought to Parkinson’s in his past episodes, was missed.
Want to get a more positive ostomy awareness message on TV and social media? Share UOAA’s Ostomy Public Service Announcement.

 how they are doing and to never forget that they are going through similar things,” Gonzalez says. He received 12 sessions of chemotherapy for six months. While in the hospital for treatment during the Christmas Holiday Gonzalez, who is an advocate and speaker for father engagement in K through 12 education and active in several area PTA’s where he raised two children, had an idea to bring some cheer to fellow patients by having local children draw cards of support to his fellow patients.
how they are doing and to never forget that they are going through similar things,” Gonzalez says. He received 12 sessions of chemotherapy for six months. While in the hospital for treatment during the Christmas Holiday Gonzalez, who is an advocate and speaker for father engagement in K through 12 education and active in several area PTA’s where he raised two children, had an idea to bring some cheer to fellow patients by having local children draw cards of support to his fellow patients. On June 25, 2021, he was taken off the TPN and underwent a successful reversal surgery to repair his intestines, clean up scar tissue, and remove the stoma.
On June 25, 2021, he was taken off the TPN and underwent a successful reversal surgery to repair his intestines, clean up scar tissue, and remove the stoma.
 Shoes should be comfortable. Wear sneakers whenever possible if that’s what you want to do. In Florida, I wear sandals with rubber soles. Up north, boots are a necessity.
Shoes should be comfortable. Wear sneakers whenever possible if that’s what you want to do. In Florida, I wear sandals with rubber soles. Up north, boots are a necessity. sport, exercise and stay away from bad habits in life. Chris played basketball and ran track, being nominated for all state in both sports. Receiving a basketball scholarship, and motivated by teachers and coaches, Chris majored in Kinesiology and Science from The Master’s University and became a teacher.
sport, exercise and stay away from bad habits in life. Chris played basketball and ran track, being nominated for all state in both sports. Receiving a basketball scholarship, and motivated by teachers and coaches, Chris majored in Kinesiology and Science from The Master’s University and became a teacher. As time went on and recovery was underway, Chris set a goal to run a 5k. Not able to keep up with his wife, she encouraged him to walk, jog, and run. Hydration was always important as part of Chris’ races, but not having a colon taught him he had to be even more diligent about it. During
As time went on and recovery was underway, Chris set a goal to run a 5k. Not able to keep up with his wife, she encouraged him to walk, jog, and run. Hydration was always important as part of Chris’ races, but not having a colon taught him he had to be even more diligent about it. During