A couple’s story of Crohn’s disease, caregiving, and family
Our battle with Crohn’s disease began back in the spring of 2006, one week after we started dating in high school. I was 16, and my now husband, Chris, was 17. We first met each other on the tennis court a few years before this- a love we still share to this day. Being just 16 and surrounded by a relatively healthy family, I had never experienced the wrath of any chronic illness, personally or by association. Chris had also been a healthy kid, which is why he and his parents found his worsening symptoms to be so alarming. As teenagers, we didn’t yet realize he had a serious condition that would need managed for the rest of our lives.
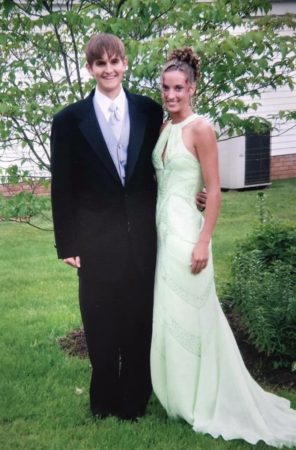
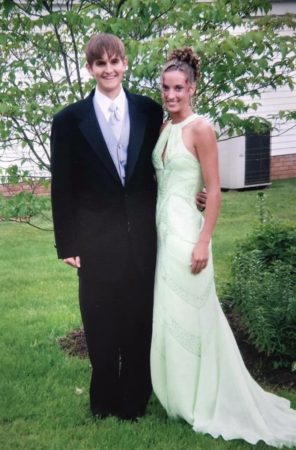
His first hospitalization happened the week after he asked me to be his girlfriend. I remember being very surprised and clueless as to why he was in the hospital. He and I practiced tennis together almost every single day, and I hadn’t noticed that anything was wrong. (To fully appreciate this journey, you have to realize that Chris does not complain about anything. Ever. He works really hard and refuses to make excuses- a trait that is both very admirable and very frustrating). Little did I know, Chris had been suffering from severe abdominal cramping, bloody diarrhea, frequent bowel movements, and weight loss for a few months, eventually landing himself a stay in the hospital. After undergoing a full GI work-up including colonoscopy and biopsies, Chris was diagnosed with ulcerative colitis (UC). He was discharged from the hospital the day before my junior prom, and he still put on a tux and attended with a smile on his face. He had joked that he was going to make it to the prom even if he had to bring his IV pole with him.
For the next year, Chris was treated with a mix of immunosuppressant medications, steroids, and blood transfusions without any improvement.
I felt so out of control. Being a patient is tough, and being a caregiver is tough- both in very different ways.
That following spring, he was referred by his local GI specialist to Cleveland Clinic for another assessment. Seeing how severe his disease was even after aggressive conservative treatment, Cleveland recommended he undergo extensive surgery by having a total proctocolectomy with ileoanal anastomosis and creation of a J-pouch with a temporary diverting ileostomy to definitively treat his UC. Chris was only 18 years old.
Chris had that first operation, which was successful, and was thankfully able to have his ileostomy reversed 3 months later. He traveled the long 4 hours back home from Cleveland and made it just in time for my high school graduation. He healed well after that second surgery and was able to begin schooling for diesel mechanics while I went to college. We got engaged before I started grad school, and he got a job working as a diesel mechanic. We then got married at 22 and 23 years old, excited to be finishing up with school and moving back home to start our adult lives. Unfortunately, for the next couple of years, he continued to have a slow progression of the same symptoms he was experiencing before his J-pouch surgery, meaning more severe abdominal cramping, bloody diarrhea, very frequent bowel movements, and weight loss. In addition to these symptoms, he developed a new complication: perianal fistulas. These symptoms persisted, leading to another scope and biopsies confirming a new diagnosis of Crohn’s disease.
Following this new diagnosis we were referred back to Cleveland Clinic for more treatment, which included multiple new medications, steroids, and transfusions. While Chris’s J-pouch surgery would have been somewhat curative for ulcerative colitis, it made it harder to effectively manage his Crohn’s. Chris continued to have this active disease in a surgically constructed reservoir (i.e. the J-pouch) making his condition, and the accompanying complications, very difficult to treat. No matter what medications he tried or how high the dosage, his health continued to deteriorate.
Over the next several years, Chris’s body went on to form a complex network of fistulas, which required multiple procedures for seton placement. He had tried hyperbaric oxygen therapy to help with the healing of his external fistulas and wounds. Unfortunately this treatment did not work.
Our kids have also been involved in everything concerning Chris’s ostomy, particularly in the beginning when it was new.
He experienced constant leakage and stool draining from multiple holes. This had become a nuisance for Chris. He also developed strictures at the inlet of the J- pouch which then resulted in endless ileoscopies for dilation to prevent obstruction. He had spontaneous bleeding due to the inflamed and ulcerated state of his intestines. There had been instances where Chris would start hemorrhaging a few hours after having a scheduled ileoscopy, causing us to rush to the ER in the middle of the night for an emergency ileoscopy to stop the bleeding. This happened on a couple of different occasions, leading to more hospital admissions and ICU stays for low hemoglobin and low blood pressure.
 I started to panic with every procedure, wondering if everything would go routinely or if we would be surprised with unexpected problems.
I started to panic with every procedure, wondering if everything would go routinely or if we would be surprised with unexpected problems.
By this time, we were traveling to Cleveland every 2-3 months for scopes and appointments, which became extremely mentally and physically exhausting for both of us. While I realize I can never begin to understand the excruciating pain Chris was experiencing, I was sort of in my own kind of emotional pain in seeing the person I love the most in this world suffer from such an awful disease. While Chris remained totally collected and level headed with each added layer of dread, I was having a hard time sitting back and watching it all happen, knowing there was absolutely nothing I could do but hold his hand in this never-ending nightmare.
I felt so out of control. Being a patient is tough, and being a caregiver is tough- both in very different ways. Luckily, our bond as a couple was already very strong, and we became more solid with each piece of bad news. It had gotten to the point where we would almost laugh about things, because what else was there to do? If we didn’t laugh, we’d cry, and we could not start that.
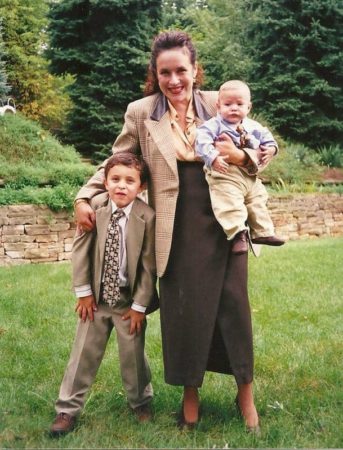
Something we were blessed with (other than our awesome marriage and a side of humor) was the love of an extremely supportive family. It was very difficult to navigate Chris’s condition as it was, but we had also been going through this while starting a family of our own and both working full time. Not to mention Chris was working a manual labor job while enduring all this misery.. can you imagine? My parents, brother, and sister-in-law stepped in to take care of us, our two small kids, and two pups whenever we needed them. They were available at a moment’s notice whether it was to watch our kids while we were in Cleveland or to help with things around the house that we just physically couldn’t get around to doing. It truly took a village to make sure everything and everyone was cared for, and we can’t even begin to express the love and appreciation we have for them. They always showed up, and having that safety net of support was so valuable, especially during that time in our lives.
Since Chris had tried and failed countless conservative treatments over the course of several years, it was then recommended he have surgery for a diverting ileostomy so that his J-pouch and fistulas could have a chance to rest and heal. Chris was not exactly thrilled with the thought of having an ileostomy, but he had run out of treatment options without any promising new therapies on the horizon. Knowing that an ileostomy was going to be a potential end result based on previous discussions with his care team, Chris was able to process his thoughts and emotions surrounding the upcoming surgery. Honestly, I think having the time to mentally prepare for such a surgery was a huge benefit in how we were all able to cope moving forward.
He had the surgery for a diverting ileostomy in January of 2020, just before the pandemic. We had hoped that he would improve with this surgical intervention, but his fistulas continued throughout that following year. He also developed a pyoderma, which is a large and painful ulcer, on his abdomen right beside his new stoma. As a result of this and the relentless fistulas and strictures, his doctors recommended he have another surgery, a major surgery, to hopefully improve his quality of life. So, one year after receiving his diverting ileostomy, Chris had an abdominoperineal resection (APR) operation. In this long, 8 hour surgery, he had his J-pouch, anus, and perianal fistulas removed. This surgery also meant that his ileostomy would be permanent without the option of ever reversing it. It would be a part of him for the rest of his life.
Our focus is on making something positive out of something that could easily seem like a burden or embarrassment.
It has now been 3 years since his APR surgery and permanent ileostomy, and Chris is healthier than ever (Shout out to the wonderful surgeons and specialists at Cleveland Clinic! We’re so very thankful for you). While the initial thought of living with an ostomy seemed daunting for Chris and for me, we have come to really appreciate everything it’s done for us. Cleveland visits are now just once a year instead of every 3 months, and Chris is only on one medication for therapeutic management. His ostomy is functioning very well and hasn’t given him any problems. Chris can change his ostomy appliance so quickly that it doesn’t even seem like an inconvenience.
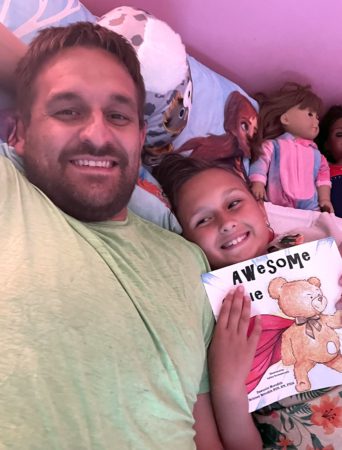
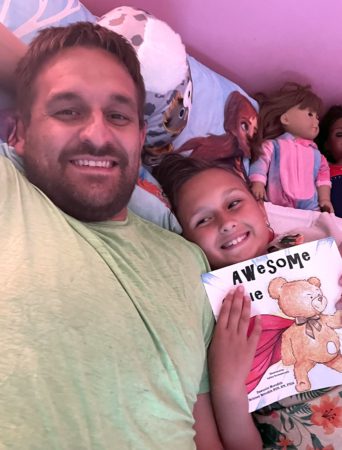
Our kids have also been involved in everything concerning Chris’s ostomy, particularly in the beginning when it was new. They have grown up seeing him do bag changes and have loved helping him get all of his supplies ready, and we welcome their questions with age appropriate answers. They were too young to remember how sick their dad was, but we don’t dwell on that part.
Our focus is on making something positive out of something that could easily seem like a burden or embarrassment. They are now 9 and 6 years old and are not ashamed that their dad wears a bag on his belly. When our daughter was in second grade, she actually took it upon herself to read “Awesome Ollie” to her class so she could educate her friends on what an ostomy is (this is an AMAZING kid friendly book we had used to prepare our kids for Chris’s ostomy surgery).
We were very impressed with her confidence and maturity to be able to share this information with a class full of kids. It was all her idea.
We are so grateful for this ostomy and the freedom it has given us. It’s like we have a new lease on life! Chris’s positive attitude throughout this entire ordeal has been such a blessing as well. He has never let his disease dictate his life, and there is so much to be said about that. Chris will gladly talk about his experiences if it means helping someone that is struggling with a similar situation, but he is not one to draw attention to himself. He never brings up how tough or terrible that part of his past was. He is such a wonderful example for our two kids, and I am proud that they will grow up seeing how great life can be despite difficult and less than optimal situations. Having an ostomy or a spouse with an ostomy is certainly an adjustment, but it doesn’t have to be a negative thing. It really is all in your mindset- just ask Chris! Even though Crohn’s is a disease that will never go away, the ostomy has been a life saver.
This is our new normal, and we are so blessed we get to experience it.




 I started to panic with every procedure, wondering if everything would go routinely or if we would be surprised with unexpected problems.
I started to panic with every procedure, wondering if everything would go routinely or if we would be surprised with unexpected problems.



 with my ostomy. After receiving my ostomy I was devastated because I was an athlete in school and didn’t know if I’d be ok to play sports or other things I loved to do again.
with my ostomy. After receiving my ostomy I was devastated because I was an athlete in school and didn’t know if I’d be ok to play sports or other things I loved to do again.

 The final year before I got surgery I had lost 40-50 pounds, had been to the emergency department countless times, as well as hospitalized 3-4 times. I ended up being super anemic and needed iron infusions as well as one blood infusion. That last year was the final straw. The summer of 2021 I ended up losing my bowels on myself 40+ times on my 20-minute drive home from work. I told my boss I couldn’t work anymore and that’s when I first heard about
The final year before I got surgery I had lost 40-50 pounds, had been to the emergency department countless times, as well as hospitalized 3-4 times. I ended up being super anemic and needed iron infusions as well as one blood infusion. That last year was the final straw. The summer of 2021 I ended up losing my bowels on myself 40+ times on my 20-minute drive home from work. I told my boss I couldn’t work anymore and that’s when I first heard about  ostomy bag. So on January 10th of 2023 I got my rectum and anus removed and they fixed my stoma prolapse. Again, the recovery wasn’t bad but this time the hospital stay was horrible. I ended up getting straight cathed three times, I had an NG tube placed because Stoma Steve wasn’t pushing food out and my drain was bothering me for the month I had it. Again, I can’t thank the subreddit r/Ostomy enough because they were who I vented to and talked to for help and coping strategies because no one in my life except them knew what I was going through.
ostomy bag. So on January 10th of 2023 I got my rectum and anus removed and they fixed my stoma prolapse. Again, the recovery wasn’t bad but this time the hospital stay was horrible. I ended up getting straight cathed three times, I had an NG tube placed because Stoma Steve wasn’t pushing food out and my drain was bothering me for the month I had it. Again, I can’t thank the subreddit r/Ostomy enough because they were who I vented to and talked to for help and coping strategies because no one in my life except them knew what I was going through.
 TPN nourishes my body with the nutrients it’s not capable of absorbing on its own. It’s delivered via a Hickman catheter in the upper left part of my chest, infusing through a pump stored in a backpack while I sleep.
TPN nourishes my body with the nutrients it’s not capable of absorbing on its own. It’s delivered via a Hickman catheter in the upper left part of my chest, infusing through a pump stored in a backpack while I sleep.
 sport, exercise and stay away from bad habits in life. Chris played basketball and ran track, being nominated for all state in both sports. Receiving a basketball scholarship, and motivated by teachers and coaches, Chris majored in Kinesiology and Science from The Master’s University and became a teacher.
sport, exercise and stay away from bad habits in life. Chris played basketball and ran track, being nominated for all state in both sports. Receiving a basketball scholarship, and motivated by teachers and coaches, Chris majored in Kinesiology and Science from The Master’s University and became a teacher. As time went on and recovery was underway, Chris set a goal to run a 5k. Not able to keep up with his wife, she encouraged him to walk, jog, and run. Hydration was always important as part of Chris’ races, but not having a colon taught him he had to be even more diligent about it. During
As time went on and recovery was underway, Chris set a goal to run a 5k. Not able to keep up with his wife, she encouraged him to walk, jog, and run. Hydration was always important as part of Chris’ races, but not having a colon taught him he had to be even more diligent about it. During 



