Why a Medical Alert ID Matters
By Ellyn Mantell with Jeanine Gleba UOAA Advocacy Manager
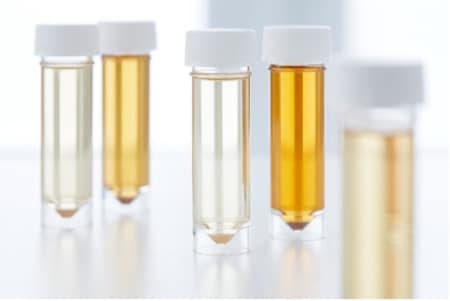
It’s a fact; ostomies and continent diversions save lives. Most people are very private about having a fecal or urinary diversion and only share information with people to whom they are most close. Living with a diversion is often considered an “invisible disability”. The concern is, what would happen with these individuals if they were in an accident, unconscious or unable to speak for themselves? They would be unable to notify an emergency responder of the unique needs of the diversion. For example, a Kock pouch is an internal pouch/reservoir that has a stoma that needs to be catheterized throughout the day to empty it. If an emergency responder were not aware of this need, it could result in over filling of the reservoir and damage to the reservoir.
There is a simple non-verbal way of communicating health issues and medical conditions in emergencies that deserves attention and should be considered. According to the Centers for Disease and Control Prevention (CDC), for personal health preparedness “help others help you” by wearing a medical alert ID bracelet or necklace engraved with important information for emergency responders and healthcare providers. By wearing a form of medical identification people living with an ostomy or continent diversion can effectively advocate for their health and safety protection when they are unable to speak up for themselves. It provides peace of mind should the worst-case scenario happen.
A real life example shared with UOAA may explain the efficacy of saving time in an emergency situation. An ileostomate was crossing the street and hit by a car. He was not terribly injured, but the force of hitting the ground caused his pouch to explode, causing the first responders to assume his abdomen had been perforated. They spent valuable time cutting clothing to find the cause of the seepage, an unnecessary waste of what could have been life-saving time. Had this gentleman been wearing a medical alert bracelet or dog tag necklace, he would have been assessed differently, and certainly more quickly.
Wearing a medical alert ID is far more effective than carrying a card in one’s wallet or handbag, or counting on another person to provide vital information. If there is an accident or incident, one may be thrown from a car, their wallet lost or removed, or one may be separated from a person who can advocate. Additionally, a family member or friend may also be incapacitated in some way, or in shock, unable to provide this lifesaving information.
It is suggested by paramedics that a medical alert bracelet be worn on the left wrist, since that is where they reach first for a pulse. A medical icon in red is an attention-grabber, but whatever form of ID you choose be sure it includes the universal medical alert symbol. Include as much information as possible and be specific. If there are medical instructions, spell them out. A sample inscription might say: Continent Urostomy Catheterize every 4-6 hours with a 1 4Fr. Catheter.
If there are other medical conditions, state them for emergency responders. Include such information as diabetes, allergies. This is no time to be vague. Include a cell phone number of a family member if there is room, and DO NOT FORGET TO ADD YOUR NAME TO THE FIRST LINE!
The most notable and recognized medical alert IDs are from the companies Medic Alert Foundation and American Medical ID. These companies can also keep on record more specific details of your medical history and current care with QR codes and ID cards in addition to the wearable ID.
For those who simply don’t like the look and style of the standard medical alert bracelet there are many more fashionable forms of ID. Other medical alert jewelry may be found on websites such as Lauren’s Hope, and Meridian Medical/Ostomy Supply Company sells a specific bracelet for ostomies. Although first responders tend to look for medical alert bracelets, for those who don’t want to wear jewelry, there are other types of IDs available including: Apple Watch slides, dog tags, and cell phone tags. Your ostomy nurse, primary care physician’s office and most pharmacies can also provide guidance.
Some people may be uncomfortable wearing something that tells others they have an ostomy or continent diversion. Don’t let stigma stop you from being emergency-prepared! Consider if you would wear medical alert identification if you had life-threatening allergies. When it comes to one’s health, it should never be associated with shame.
Ostomies and medical alert IDs go hand in hand saving lives.
Disclaimer: UOAA does not endorse particular products, manufacturers, or suppliers.





 40 vendors will be there to visit with you and share any new products they are offering, services they provide, clothing and accessories available in today’s market, and much more. We’ll be serving a complimentary boxed lunch on Friday before the Exhibit Hall closes at 1pm for you to enjoy.
40 vendors will be there to visit with you and share any new products they are offering, services they provide, clothing and accessories available in today’s market, and much more. We’ll be serving a complimentary boxed lunch on Friday before the Exhibit Hall closes at 1pm for you to enjoy.
 UOAA’s 9th National Conference. Stay a few days earlier or after the conference and enjoy what the Resort has to offer with family and/or friends.
UOAA’s 9th National Conference. Stay a few days earlier or after the conference and enjoy what the Resort has to offer with family and/or friends.








 signing onto ten different letters that were sent to Congress many with positive results and we had several open action alerts on our advocacy platform supporting Federal legislation. We also continue to advocate with the Access and Care Coalition in our efforts with the Medical Directors from the Centers of Medicare and Medicaid Services (CMS) to make improvements to the ostomy policies and processes in particular for those beneficiaries who medically need greater quantities of products than what is allowable under the current policy. We won’t stop until this is resolved. Another example has been challenges with
signing onto ten different letters that were sent to Congress many with positive results and we had several open action alerts on our advocacy platform supporting Federal legislation. We also continue to advocate with the Access and Care Coalition in our efforts with the Medical Directors from the Centers of Medicare and Medicaid Services (CMS) to make improvements to the ostomy policies and processes in particular for those beneficiaries who medically need greater quantities of products than what is allowable under the current policy. We won’t stop until this is resolved. Another example has been challenges with