You’ve heard the myths about ostomy bags. They’re smelly. Leaky. A dreaded last resort no one would ever choose.
These myths—old, untrue, and stubborn—keep stigma alive. They tell a story that says ostomy bags are something to hide. Something to be ashamed of. Something to avoid or pity. Fueling careless jokes and bleak portrayals, the myths strip away the complexity of ostomy life and reduce it to a sad, lonely struggle.
But ostomy bags are not tragedies. They are not cheap punchlines or secrets to carry in shame. For 725,000 to 1 million people in the United States alone, ostomies are lifelines—tools of survival and symbols of strength. Ostomies make it possible for people to keep living when illness, injury, or pain have tried to take that away.
It’s time to change the conversation. Here are four things everyone should know about ostomy bags and the people wearing them.
1) Myth: An ostomy is a worst-case scenario.
Truth: An ostomy may save and improve lives in ways people don’t often expect.
Ostomy surgery is often framed as a tragedy. Some say they’d rather die than have one. Others insist they could never live like that. Others still tilt their heads with misplaced sympathy: I’m so sorry you have to wear that. Is it temporary?
Underneath these comments is the unspoken belief that an ostomy is a fate so grim, it should be avoided at all costs.
But here’s what people don’t see: An ostomy can give life back. For so many, it means meals without pain or fear. Days without the clench of needing a bathroom now. The relief of a body no longer ruled by urgency, accidents, and the constant worry that public outings will end in embarrassment.
For those with Crohn’s disease or ulcerative colitis, an ostomy may be what breaks the relentless cycle of flares, medications, and hospital stays. For those with colorectal or bladder cancer, it can be a turning point in removing disease and reclaiming the body. For these and so many other people—those with diverticulitis, traumatic injuries, congenital conditions—an ostomy can be a doorway to fully living.
This isn’t about pretending that life with an ostomy is perfect. It’s about telling the whole truth. Yes, an ostomy can change things. Yes, there may be moments of frustration, doubt, or grief. But for so many ostomates, there is also freedom, relief, and possibility.
And that is anything but the worst.
2) Myth: Ostomies are only for older people.
Truth: Ostomies are for anyone who needs them, from babies to the elderly.
When people hear the word ostomy, they may picture this: an older person in a hospital gown, frail and confined to a bed. But ostomies aren’t just for old age, and they certainly aren’t just for hospitals.
They are for living—for anyone whose body needs a different way forward.
Ostomies are for:
- The baby born with a condition requiring immediate intervention
- The toddler whose parents mastered ostomy bag changes before potty training
- The child with a backpack of homework, snacks, and ostomy supplies
- The teenager balancing WOC appointments with school, friendships, and first dates
- The new parent learning to care for a baby while relearning to care for themselves
- The professional navigating a medical curveball at the height of their career
- The grandparent chasing after grandkids, refusing to slow down
- And yes, older individuals who have lived through it all
Ostomies belong to every age and every stage of life. When we widen the lens, we find them at playgrounds and in boardrooms, at first dates and family vacations, in classrooms and grocery store aisles.
We create space for anyone with an ostomy who wonders if there’s someone out there like them. We show them the truth: no matter their age, no matter where they are in life, they are not alone.
3) Myth: No one will love you with an ostomy.
Truth: Love is so much bigger than a bag.
Many ostomates fear they’ll never find someone who sees beyond their ostomy bag. The questions linger between swipes, dates, and hesitant disclosures. When do I bring it up? How will they react? They wonder if the moment they say ostomy bag, there will be an awkward pause and silent calculation that it’s just too much.
Some wish they had fallen in love before surgery—so they wouldn’t have to explain. So the love would already be there, solid and secure. So they wouldn’t have to brace for the moment someone sees the bag and decides whether they can “handle it.”
Even those in relationships may wrestle with doubt. Will my partner still want me? Still find me attractive? Can I trust when they say that this doesn’t change anything?
An ostomy adds another layer to intimacy and relationships. Some potential partners do flinch. Some hesitate. Some don’t know what to say, or they say the wrong thing, or they give a look that stings. (This is stigma in action.)
But love—the kind worth having—is not that fragile. It is not scared of an ostomy bag. And there’s more of that love out there than people think.
People find love at every stage of their ostomy journey. Some before surgery, with partners who sit beside them in hospital rooms, proving that for better or worse isn’t just a phrase. Others after, when they are finally well enough to show up fully in their lives—embracing a love that doesn’t come despite the ostomy, but because of the space it created for healing and wholeness.
Bag or no bag, love is about connection—truly seeing and being seen. And the partners of ostomates prove every day that it’s actually not about looking past the bag at all. They see the bag. They honor it. Not as an obstacle, but as a mark of their partner’s resilience, vulnerability, courage, and strength.
And those are qualities worth loving.
4) Myth: You can tell if someone has an ostomy bag.
Truth: With the right products and care, ostomies often go unnoticed.
People with ostomies are everywhere: at work, at the gym, on dates, in line at the coffee shop. Chances are, most people have met someone with an ostomy without ever realizing it. They’ve stood next to them, shook their hands, shared a laugh—and never knew.
That’s because ostomy bags are not what people think. They’re not open or exposed. They’re not constantly leaking odor or waste in public. In fact, many ostomy bags don’t even resemble the crinkly, medical-looking pouches of the past. Today, there are options designed for discretion and comfort. Sight, sound, scent? All covered. Most of the time, an ostomy is invisible unless the person wearing it chooses to share.
For those who do experience leakage or complications with their ostomy, or just prefer an extra layer of discretion, there are options. A change in products or routine, a wardrobe shift—adjustments that restore comfort and control because people with ostomies aren’t meant to live in constant worry. If someone wants discretion, it can be theirs.
The truth about ostomy myths
Ostomy myths don’t just mislead; they shape lives. They seep into conversations, assumptions, and even the way people see themselves. They chip away at confidence, making it harder for those with ostomies to fully show up in their lives. They feed fear in those facing surgery, delaying care and prolonging suffering. And for everyone else, they can reinforce the dangerous idea that some bodies are more worthy than others.
An ostomy bag doesn’t shrink a person’s worth. It doesn’t make them any less strong, less capable, or less deserving of love and respect.
Because a person with an ostomy is not their bag. No matter who they are—no matter when, how, or why they got their ostomy—they are so much more.
Coloplast develops products and services that make life easier for people with intimate healthcare needs. Working closely with the people who use our products, we create solutions that are sensitive to their special needs. Our business includes ostomy care, continence care, advanced wound care, interventional urology, and voice & respiratory care.
Follow Coloplast on Instagram, Facebook, and YouTube, or visit us online at https://www.coloplast.us/
Author’s note: This blog primarily uses the term “ostomy bag” to reflect how the author describes her own pouching system—a functional, everyday part of her life. While the intent is to reclaim the word “bag” from its negative associations, we recognize that others advocate for alternative terms like “ostomy pouch.” Whenever possible, please ask those with ostomies about the language they prefer.
Editor’s note: This blog is from a UOAA digital sponsor, Coloplast. Sponsor support along with donations from readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.

 experts, and health communication experts. This guide is freely available
experts, and health communication experts. This guide is freely available 
 people to remember that no one knows that the noises came from the ostomy. It is ok to say nothing (low disclosure). It is also ok to say: “Excuse me, I have an ostomy pouch and sometimes it makes noises” (medium disclosure).
people to remember that no one knows that the noises came from the ostomy. It is ok to say nothing (low disclosure). It is also ok to say: “Excuse me, I have an ostomy pouch and sometimes it makes noises” (medium disclosure).
 Shoes should be comfortable. Wear sneakers whenever possible if that’s what you want to do. In Florida, I wear sandals with rubber soles. Up north, boots are a necessity.
Shoes should be comfortable. Wear sneakers whenever possible if that’s what you want to do. In Florida, I wear sandals with rubber soles. Up north, boots are a necessity.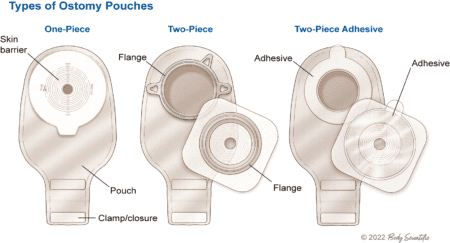 The ostomy nurse had a lot of information to cover in a short period, and she thought all of it was important. Afraid of failing, I was certain that I was going to make terrible mistakes. I doubted my ability to do any of this.
The ostomy nurse had a lot of information to cover in a short period, and she thought all of it was important. Afraid of failing, I was certain that I was going to make terrible mistakes. I doubted my ability to do any of this.

 For me, I plan to get back to my full fitness routine once I am fully recovered. I already feel healthier than I have for so many years. But I know I still have a lot of learning to do… from
For me, I plan to get back to my full fitness routine once I am fully recovered. I already feel healthier than I have for so many years. But I know I still have a lot of learning to do… from 



