Have questions about a urostomy? Worried that getting one will change your life dramatically? Terrified of the idea of one and wondering what people will think?
By Robin Glover
Don’t worry. These are normal feelings. Nobody likes the idea of getting a urostomy – at first. However, if you talk to people who’ve had one a while, they’ll tell you how much it’s improved their lives, and likely saved it.
So feeling a little apprehensive (or a lot) is completely expected. But getting a urostomy should not hold you back from living the life you’ve always wanted. Will it change your life? Yes, but likely for the better compared to past bladder issues.
What Is A Urostomy?
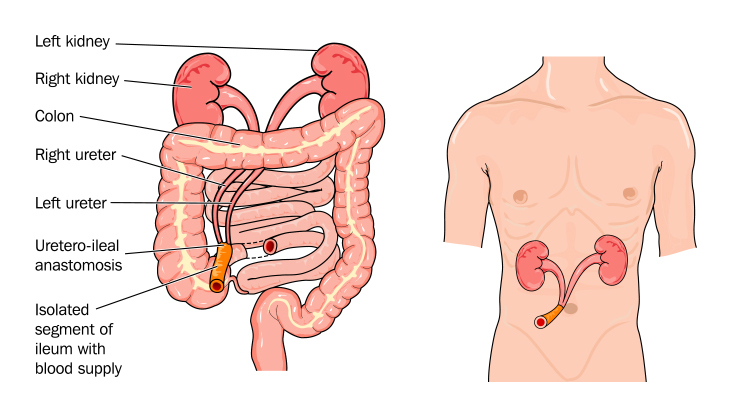
A urostomy allows urine to leave the body without the need of a bladder. Also known as an ileal conduit, it is a surgically-created pathway that channels urine through the intestine to an opening on the abdomen. This opening, known as a stoma, is covered by an external pouching system that collects the liquid.
 Why Do People Need A Urostomy?
Why Do People Need A Urostomy?
People need a urostomy because their bladder has either been removed or doesn’t function properly. This is most often due to bladder cancer, but can also be the result of an injury or disease. In other cases, people are born with a non-functioning bladder and benefit from a urostomy their entire lives.
Is A Urostomy Gross?
No. Not at all. They do not cause an odor, and most people won’t even know if someone has one. Getting a urostomy is often a life-saving procedure that allows people to resume their everyday lives. Most people find it much easier and more sanitary to have a urostomy than deal with an incontinent bladder.
Will A Urostomy Affect My Daily Life?
There will be some adjustments after surgery, but most people who get a urostomy can usually do more things than they could before. You won’t need to worry about the embarrassment of having an accident in public or always needing to know where the nearest bathroom is. But most of all, you’ll be able to live a longer and healthier life.
Is A Urostomy The Same As A Colostomy?
While they share similar mechanisms in how they function, a urostomy helps people with bladder incontinence. A colostomy helps people with stool incontinence. Both use a pouching system to collect what comes out, and both are sanitary and safe without any odor when closed. Urostomy pouches have a tap or valve to allow the urine to be drained quickly and easily. Overnight options are available for nighttime drainage convenience.

How Many People Have A Urostomy?
You are not alone. An estimated 725,000 to one million people in the United States have an ostomy or continent diversion. Colostomy and ileostomy surgery are the most common ostomy types but many thousands of people of all ages and backgrounds have a urostomy or urinary diversion. For a bit of inspiration read a few of their patient stories on our blog.
How Will A Urostomy Change My Diet?
You can eat whatever you want when you have a urostomy. Of course, this is barring specific restrictions from your doctor or other dietary limitations unrelated to having a urostomy. But, in general, there are no restrictions to what you can eat with a urostomy but information on the importance of hydration and other good health practices are covered in our ostomy nutrition guide.
What Is A Continent Urostomy?
A continent urostomy involves a surgically formed internal reservoir that allows control of when urine is released from the body. It usually involves a catheter that’s inserted into the stoma. Continent urostomies can also be routed through the urethra so urine is released from the body in a more typical fashion. Check out our Continent Urostomy Guide for more information.
Does A Urostomy Decrease Life Expectancy?
The answer is no. Urostomy surgery is a way to help people live longer and more fulfilled lives. So if you’ve been told you need a urostomy, as much as you might not think so right now, you’ll probably be glad you had it.
These are probably just a few questions you have about a urostomy. Luckily, there are people all over the world happy to help you. First of all, your Wound, Ostomy, and Continence (WOC) nurse is there to teach and help you. But practical advice and emotional support are always just a click away in online communities and by finding a UOAA Affiliated Support Group near you. Just remember that only your doctor and WOC nurse know the unique circumstances of your condition.
For more information on urostomies, please visit our Urostomy Facts Page.
Robin Glover is a writer based in the Houston area. He has a permanent ostomy after being diagnosed with Crohn’s Disease in 2017.



 Without an
Without an 
 So, what can I do now that I have a urostomy?
So, what can I do now that I have a urostomy? There are so many other things I have been able to do since my
There are so many other things I have been able to do since my 
 nurses) would recommend 3‐5 days of wear time. What I would definitely advise against is waiting until you HAVE to change due to a leak. Before you realize you have a problem, waste is coming into contact with your peristomal skin, and that may lead to skin damage. Above all, you want to keep your skin healthy, happy and intact. So when would my daily activity impact my wear time? Again it’s moisture math! I mentioned earlier that I like to swim and jacuzzi; a quick dip for an hour or so is very different than a big day out that involves being in a wet bathing suit all day. If I am planning a big day out on the water, in the pool, at a beach or waterpark, I figure that in to my changing schedule. For example if day one was Thursday, and day three is a big day out involving water, when I get home, I’ll typically shower and do a full change.
nurses) would recommend 3‐5 days of wear time. What I would definitely advise against is waiting until you HAVE to change due to a leak. Before you realize you have a problem, waste is coming into contact with your peristomal skin, and that may lead to skin damage. Above all, you want to keep your skin healthy, happy and intact. So when would my daily activity impact my wear time? Again it’s moisture math! I mentioned earlier that I like to swim and jacuzzi; a quick dip for an hour or so is very different than a big day out that involves being in a wet bathing suit all day. If I am planning a big day out on the water, in the pool, at a beach or waterpark, I figure that in to my changing schedule. For example if day one was Thursday, and day three is a big day out involving water, when I get home, I’ll typically shower and do a full change.



