Since its inception United Ostomy Associations of America, Inc (UOAA) has supported and welcomed members living with a urostomy (ileal conduit) or urinary diversion as a result of bladder cancer and related conditions.
Urostomy surgery is explained in a page from UOAA’s Living with a Urostomy Guide
May is Bladder Cancer Awareness Month. The American Cancer Society’s estimates about 82,290 new cases of bladder cancer United States for 2023 and about 16,710 deaths from bladder cancer (about 12,160 in men and 4,550 in women)
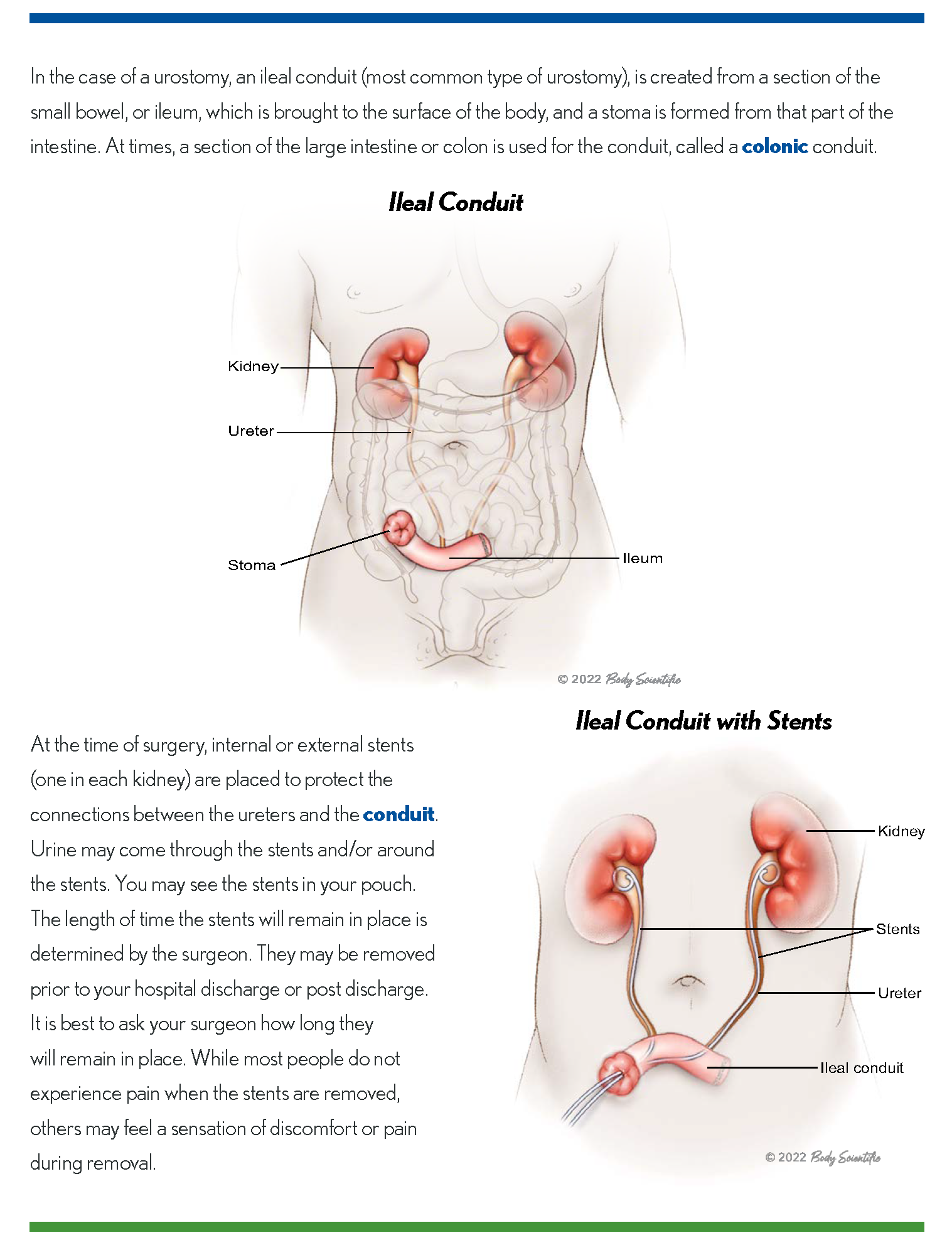
While this common cancer is most often treated without radical surgery a urologist may suggest bladder removal surgery to stop the cancer if a bladder tumor reaches the deeper muscle wall or resists other therapy. A urinary diversion is needed to replace the bladder. This involves using parts of the intestines to allow urine to pass from the kidneys to either an internal urinary reservoir pouch such as Indiana Pouch or a neobladder or an external ileal conduit, when a stoma is formed. An ostomy pouch is worn over the stoma to collect urine.
With surgery comes new things to learn and adjust to in order to achieve the quality of life you were used to before bladder cancer.
UOAA has over 270 Affiliated Support Groups around the United States. Bladder cancer survivors attend many of them and also serve as volunteers and leaders. Peer support and preparation can put you on the path to success in what may be a challenging time both emotionally and physically.
We recognize that those with an ileostomy, colostomy and various gastrointestinal disorders may dominate public conversations and education about living with an ostomy. Please know that the voices of urostomates and those with a urinary diversion are also supported and amplified by UOAA.
A new Living with a Urostomy Guide was launched this year and is available for free online. Created by ostomy nurses with input from a urostomy patient and a leading urologist, this trusted resource is vital to anyone who has or may have to have this life-saving surgery.
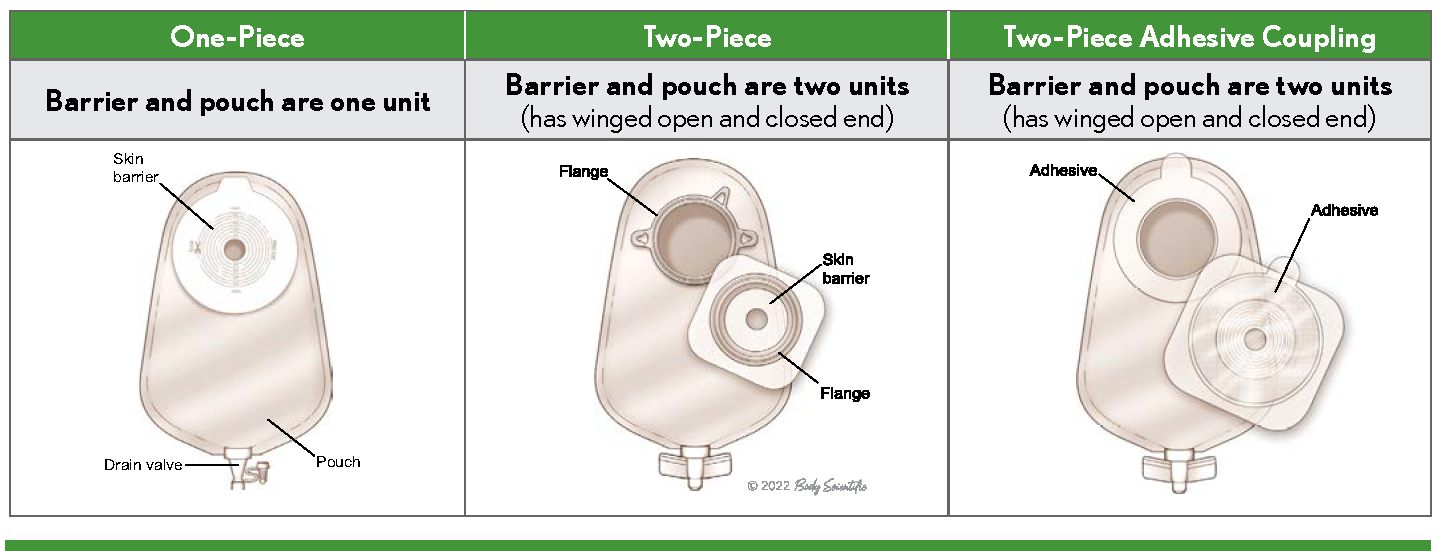
Learn about the unique aspects of a urostomy pouch and options that help improve sleep for urostomates like a night drainage bag.
Ostomy.org is also home to a guide on continent urostomies and other specific considerations.
UOAA advocates on a national level for all people living with an ostomy or continent diversion. Consider taking out a National Individual Membership to help amplify our voices and receive special member benefits along the way.
Check out our many self-advocacy tools designed to help you know what to expect and to take control of your healthcare. Learn that you matter and become a champion for the Ostomy and Continent Diversion Patient Bill of Rights.
It’s important to learn the facts about living with an ostomy. After the healing period outlined by your surgeon you can swim, bathe, travel, and embrace a new normal life. Reading patient stories from both the male urostomy patient and female bladder cancer survivor perspectives are also helpful.
Seize any opportunity to meet other urostomates. UOAA’s 2023 National Conference in August will feature special sessions and meet-up opportunities for people living with a urostomy.
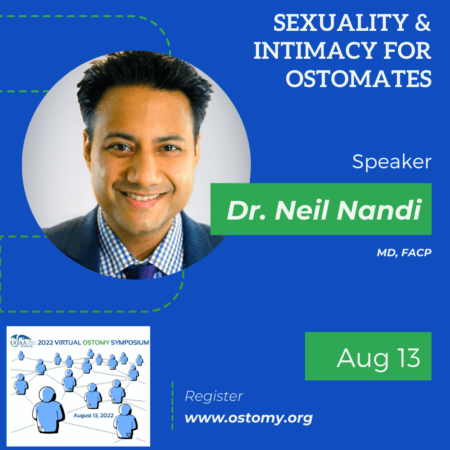
People living with an urostomy as a result of bladder cancer may experience unique sexual issues. Consult with you doctor but also learn about some common issues in our sexuality and intimacy guide.
Misinformation and stigmas surrounding both ostomy surgery and bladder cancer still exist. Nonprofits like Bladder Cancer Advocacy Network (BCAN) and UOAA are working to improve quality of life with support and information. Bladder cancer survivors are an important part of UOAA, join with us to create a better tomorrow.

 (DDNC) and the Safe Step Act Coalition where we share common goals and work together to achieve them. For example, the DDNC’s mission is to work cooperatively to improve access to and the quality of digestive disease health care in order to promote the best possible medical outcome and quality of life for current and future patients. Although UOAA is unable to have its own “ostomy” lobby days or fly-ins on the Hill (due to financial limitations), we are an important part of the annual DDNC Spring Public Policy forum. Ostomy advocates join forces with other digestive disease advocates to meet with Congressional staffers to share their stories and ask for support of our federal legislative priorities. These coalitions submit joint letters of requests or support/opposition to Congressional leaders and key regulatory decision-makers. An example of power and strength in numbers is the Safe Step Act Coalition which now comprises 215 patient organizations all advocating for passage of this important piece of legislation!
(DDNC) and the Safe Step Act Coalition where we share common goals and work together to achieve them. For example, the DDNC’s mission is to work cooperatively to improve access to and the quality of digestive disease health care in order to promote the best possible medical outcome and quality of life for current and future patients. Although UOAA is unable to have its own “ostomy” lobby days or fly-ins on the Hill (due to financial limitations), we are an important part of the annual DDNC Spring Public Policy forum. Ostomy advocates join forces with other digestive disease advocates to meet with Congressional staffers to share their stories and ask for support of our federal legislative priorities. These coalitions submit joint letters of requests or support/opposition to Congressional leaders and key regulatory decision-makers. An example of power and strength in numbers is the Safe Step Act Coalition which now comprises 215 patient organizations all advocating for passage of this important piece of legislation!


 Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary
Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary 
 from wonderful WOC nurses, experienced ostomates, amazing doctors and dedicated advocates.
from wonderful WOC nurses, experienced ostomates, amazing doctors and dedicated advocates. The event will come to a close with a special presentation from Magen Cherry, a j-poucher and winner of the 2007 Miss Texas USA competition. She uses her platform to share encouragement and bring hope to fellow ostomates and j-pouchers coming to terms with their new reality. Fun fact: Magen had a colonoscopy three days after being crowned Miss Texas USA!
The event will come to a close with a special presentation from Magen Cherry, a j-poucher and winner of the 2007 Miss Texas USA competition. She uses her platform to share encouragement and bring hope to fellow ostomates and j-pouchers coming to terms with their new reality. Fun fact: Magen had a colonoscopy three days after being crowned Miss Texas USA!


 being admitted within the first 90 days post operatively [1]. This is one of the highest rates of readmission when compared to other types of surgery. The most common cause for re-admission is dehydration, at approximately 40% of post ileostomy readmissions [2]. We also know that 84% of ostomy patients develop skin issues. The causes of these can be chemical, mechanical, or microbial, and possibly avoidable. Ostomates also have significantly increased healthcare costs, especially when affected by peristomal skin complications, and leakage [2]. It is known that 25% of ostomates develop renal failure within two years. The complications these patients encounter require 7x more outpatient visits than the average patient. And 29.1% of ostomates experience readmission which costs approximately $16,000 per patient [1]. These statistics show that specialized care for these patients is imperative to improving patient outcomes in this patient population.
being admitted within the first 90 days post operatively [1]. This is one of the highest rates of readmission when compared to other types of surgery. The most common cause for re-admission is dehydration, at approximately 40% of post ileostomy readmissions [2]. We also know that 84% of ostomy patients develop skin issues. The causes of these can be chemical, mechanical, or microbial, and possibly avoidable. Ostomates also have significantly increased healthcare costs, especially when affected by peristomal skin complications, and leakage [2]. It is known that 25% of ostomates develop renal failure within two years. The complications these patients encounter require 7x more outpatient visits than the average patient. And 29.1% of ostomates experience readmission which costs approximately $16,000 per patient [1]. These statistics show that specialized care for these patients is imperative to improving patient outcomes in this patient population.


