Imagine if there was a place where over forty ostomy product manufacturers, accessory makers, distributors, lifestyle experts, and related support organizations could gather with ostomy patients from around the world? Well, UOAA’s 7th National Conference Exhibit Hall is that place, and everyone is invited. It will be open August 8 and 9, 2019 at the Philadelphia 201 Hotel in the heart of Philadelphia, Pennsylvania.
People return to UOAA’s biennial national conferences not only because of the lifelong friendships, education, and social events but also because of the exhibit hall. It is a fun one-stop experience to ask questions about your favorite supplies or discover what is the latest and greatest in the world of ostomy care. Attendees have the chance to sign-up for sample products and talk one-on-one with representatives of all the major and specialty ostomy product manufacturers. Visitors often find the passionate owners and inventors of unique ostomy products on hand to introduce you to their products.

UOAA is proud to be able to provide this space for our community to gather. The conference runs Aug. 6-10, but If you can only come to our conference for one day you’ll want to consider registering for the exhibit hall days Thursday and Friday. There is even a free box lunch Friday for all those registered attendees who enter the exhibit hall. You may want to consider staying longer, however, to take advantage of the free stoma clinic, expert educational session and surgery specific meet-ups. And don’t miss social events such as the Roaring 20s Casino Night and Music Thursday and the Saturday night fashion show, desserts, and dancing. Be sure to stop by UOAA’s table where you can sign an important petition for the Ostomy and Continent Diversion Patient Bill of Rights and learn about all the upcoming events such as Ostomy Awareness Day and the Run for Resilience Ostomy 5k.

Here is a list of all the businesses and organizations exhibiting this August. Like UOAA, they are dedicated to improving the quality of life of people living with an ostomy.
11 Health and Technologies Inc.
www.11Health.com • 657-266-0570
11 Health helps people living with medical bags by combining peer-to-peer support with unique patented SmartBags that collect patient generated data for preventative care. 11 Health thinks and acts differently from all established medical bag companies because we see the patient as a patient – not an end user.
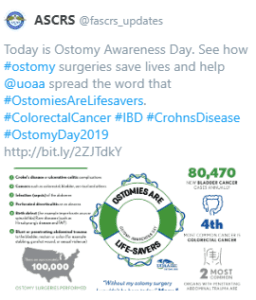
ASCRS – Colon/Rectal Surgeons
www.fascrs.org • 847-290-9184
You are invited to visit the ASCRS Booth and receive information regarding services ASCRS can provide, including patient referrals and patient education brochures. The scope of colon and rectal surgery includes the small bowel, colon, rectum and anal areas.
Avadim Health, Inc.
www.theraworxprotect.com • 877-677-2723
Avadim Health Inc. is the Bionome Life Science company. Avadim’s flagship product Theraworx® Protect is a topical solution that supports the skin’s outer most layer, the stratum corneum, while remaining Non-Toxic and Safe.
B Braun Medical
www.bbraunusa.com • 800-227-2862
B. Braun Medical Inc. develops, manufactures, and markets innovative medical products and offers ostomy products including Flexima® 3S two-piece appliance with a unique guiding system and a High Output System. The myosto™ resource offers ostomates the ability to request product samples and educational resources on the website. Visit www.bbraunusa.com and www.myosto-mylife.com
Byram Healthcare
www.byramhealthcare.com • 800-227-2862
Byram is the leading service and solutions provider of disposable medical supplies delivered directly to the home while conveniently billing insurance plans. We provide convenience, affordability and choice™ to make a positive difference in the lives of the people we serve.
Calmoseptine, Inc.
www.calmoseptine.com • 714-840-3405
Calmospetine® Ointment protects and helps heal skin irritations from moisture such as urinary and fecal incontinence. It is also effective for irritations from perspiration, wound drainage, fecal and vaginal fistulas and feeding tube site leakage. Calmoseptine® temporarily relieves discomfort and itching. Free samples at our booth!
Cancer Support Community
www.cancersupportphiladelphia.org
Cancer Support Community is a leader in cancer support, and is the largest cancer support organization in the world that provides 100% free services and programs for individuals and families impacted by cancer. The Community serves those with cancer, who have a family member or friend with cancer and who have lost a loved one to cancer.
Celebration Ostomy Support Belt
www.celebrationostomysupportbelt.com • 413-539-7704
Our ostomy Celebration Belt systems are designed to protect your dignity while allowing you to lead an active life. Learn how to measure for a correct fit, get wear and care information, and order your belt with confidence.
Colo-Majic Enterprises
www.colomajic.com • 866-611-6028
Colo-Majic® Flushable Liners are designed to be inserted into a two piece closed end pouch system to collect colostomy/ileostomy output. Liners will keep your pouch clean allowing for reuse and makes output disposal quick and easy.
Coloplast
www.coloplast.us • 888-726-7872
Coloplast develops products and services that make life easier for people with very personal and private medical conditions. Working closely with the people who use our products, we create solutions that are sensitive to their special needs. Our business includes ostomy care, interventional urology, continence care, wound & skin care.
ConvaTec
www.convatec.com • 800-422-8811
At ConvaTec, we exist to improve the lives of the people we touch and are committed to helping people living with an ostomy live the life they want with more confidence and freedom. Our me+ program gives you the support, insights and products you need. For more information, visit convatec.com.
Crohn’s & Colitis Foundation
www.crohnscolitisfoundation.org 888-694-8872
The Crohn’s & Colitis Foundation is dedicated to finding cures for Crohn’s Disease and ulcerative colitis, and to improving the quality of life of children and adults affected by these diseases. The Foundation is at the forefront of research in inflammatory bowel diseases in addition to educating, supporting, and empowering patients and caregivers.
Edgepark
ww.edgepark.com • 800-321-0591
Edgepark is a leading provider of home-delivered, disposable medical products. We specialize in ostomy, wound care, urological, incontinence, diabetes and more, offer comprehensive insurance options and provide free nationwide delivery. To learn how we can help meet your supply needs, please call 800-321-0591 or visit www.edgepark.com.
Friends of Ostomates Worldwide
www.fowusa.org • 502-909-6669 • info@fowusa.org
Friends of Ostomates Worldwide-USA is a volunteer-run, non-profit organization that collects donated ostomy supplies from individuals and organizations in the United States and sends them and educational materials at no cost to ostomates in need around the world.
Girls With Guts
www.girlswithguts.org • info@girlswithguts.org
The vision of Girls With Guts is to establish a national support network that assists women with IBD and/or ostomies in their search for community, acceptance, and empowerment. This rapidly growing sisterhood helps to ensure that no woman will ever feel isolated by her disease.
Hollister Incorporated
www.hollister.com • 888-740-8999
At Hollister Incorporated, we are dedicated to delivering the highest standard of quality in medical products and services, and each member of the Hollister team is committed to making a difference in the lives of people who use our products and services.
Hy-Tape Int.
www.hytape.com • 800-248-0101
Hy-Tape’s latex-free, waterproof, zinc oxide-based adhesive is soothing to delicate skin, and removes without compromising skin integrity. Our tape is perfect for extended ostomy wearing time, adhering securely so the end user can resume normal activities such as walking, exercising, bathing and swimming without worry of detachment.
KEM Enterprises, Inc.
www.kemonline.com • 616-676-0213
KEM Enterprises, Inc. manufactures the Osto-EZ-Vent.® The Osto-EZ-Vent® is the unique venting device designed for any Ostomy pouch, which allows quick, discreet release of air pressure. Invented by an Ostomate, the OEV™ gives the wearer complete control and confidence to lead an active life. Medicare code A4366. Visit us at kemOnline.com.
Marlen Manufacturing
www.marlenmfg.com • 216-292-7060
Since 1952, Marlen has been a leading innovator in ostomy care. Offering an extensive line of one-piece and two-piece systems for Ileostomies, Colostomies and Urostomies, Marlen has always strived to provide the highest quality products while meeting the comfort and security needs of our customers. Visit our website at www.marlenmfg.com
McKesson Patient Care Solutions
www.mpcs.mckesson.com • 855-404-6727
From doctor to doorstep, McKesson Patient Care Solutions provides healthcare that fits into your everyday life. With online support to answer all your questions, a team of customer service Reps to help you choose the right supplies, and fast, convenient shipping right to your door.
No You Cant’cer Foundation
www.noyoucantcerfoundation.org • 609-464-4647
The No You Cant’cer Foundation is a nonprofit organization working to dispel the negative stigmas surrounding ostomy bags and colorectal cancer while inspiring through song. By nationally distributing informational pamphlets and creating her awareness ribbon necklaces, cancer survivor and ostomate Melissa Marshall aims to help everyone say No You Cant’cer.
Nu-Hope Labs
www.nu-hope.com • 800-899-5017
Nu-Hope manufactures ostomy devices, accessories, belts, barriers and adhesives. We specialize in custom molded pouches and custom ostomy/hernia belts. Other highlights are our oval convex pouches, and stoma wafer hole cutters. Check out the Nu-Comfort belt and new for 2019, our moldable extended wear barrier. Don’t forget the Fun Run/Walk!
Oley Foundation
www.oley.org • 518-262-5079
The Oley Foundation is a non-profit organization providing information and support to those sustaining themselves on home infused and/or tube fed nutrition. Outcome data demonstrates that those connected to Oley have better outcome: significantly higher quality of life, less reactive depression, and a lower incidence of catheter-related sepsis.
Ostomy Canada Society
www.ostomycanada.ca • 888-969-9698
Ostomy Canada Society is a non-profit volunteer organization dedicated to all people with an ostomy and their families, helping them to live life to the fullest through support, education, collaboration and advocacy. www.ostomycanada.ca
Parthenon Co., Inc.
www.parthenoninc.com • 800-453-8898
Family owned and operated for over 50 years. The Parthenon Company is a manufacturer and discount retailer specializing in ostomy supplies servicing customers throughout the United States.
Philadelphia Ostomy Association
www.philaost.org
The Philadelphia Ostomy Association was established in 1949 as the Colostomy Ileostomy Rehabilitation Association. As time went on and Urostomy surgery was developed, we changed our name to the Philadelphia Ostomy Association to support all types of ostomates.
Pouch Place
www.pouchplace.com • 865-531-1285
Nurse owned and managed ostomy care and supplies. For more than 27 years the Pouch Place has offered a complete selection of ostomy, wound care and incontinence supplies treating each patient’s needs with thoughtful and respectful care from two store front locations and an online store serving patients nationwide.
Pull-thru Network, Inc.
www.pullthrunetwork.org • 309-262-0786
Pull-thru Network, Inc (PTN) is a volunteer-based non-profit organization dedicated to providing information, education, support and advocacy for families, children, teens and adults who are living with the challenges of congenital anorectal, colorectal, and/or urogenital disorders and any of the associated diagnoses.
Quality Life Association, Inc.
www.qla-ostomy.org • 662-801-5461
The Quality Life Association, Inc. (QLA) is a non-profit nationwide association aimed at meeting the special needs of the continent ostomate and to educate others on the latest advances in ostomy options.
Safe n Simple
www.sns-medical.com • 844-767-6334
Safe n simple is an innovator that develops and markets a full line of high quality, cost-effective ostomy accessory products. The patented Peri-Stoma Cleanser and Adhesive Remover wipes are their most popular product. Now offering Security Hernia/Ostomy Support Belts.
Sanitary Ostomy Systems, Inc.
www.sanitaryostomysystem.com • 805-441-6708
Discover Our Exclusive Pouch-Emptying Systems For Use At Home And Everywhere Else. THE SOS KIT: Compresses pouch contents into a detachable, disposable collection bag. The perfect reusable solution for ostomates & caregivers. THE TRAVELER KIT: Empties your pouch anytime, anywhere – even in your car! Completely disposable, discreet and easy.
Schena Ostomy Technologies, Inc.
www.ostomyezclean.com • 239-263-9957
The revolutionary EZ-Clean Pouch system can be cleaned in less than 3 minutes. Water under pressure is dispersed via a manifold inside the pouch to provide thorough, hygenic cleansing of the pouch and stoma while sitting on the toilet. See details on how to normalize life with an ostomy online at: www.ostomyezclean.com.
Simply Beautiful
www.simplybeautifulstore.com • 304-771-1773
Wraps and Lingerie that empower women and preteens to feel more confident and reveal your true beauty while thriving with an ostomy.
Stealth Belt Inc.
www.stealthbelt.com • 800-237-4491
A Stealth Belt is an ostomy support belt that is specially designed to hold an ostomy appliance securely and discreetly. A Stealth Belt may be worn 24/7 to provide comfort and give you privacy. Stealth Belt’s great design features include, light weight fabric, a zippered pouch compartment, and a range of adjustability for ease of sizing.
Stomagienics, Inc.
www.stomagienics.com • 225-939-1460
Stomagienics Inc., was created based on an extraordinary situation involving a family member who, after having ostomy surgery, solved a plaguing issue that occurs during the ostomy pouch replacement process. We use many of his original design principles to create a revolutionary new product that will change the lives of ostomates worldwide.
Surviving to Thriving
www.elaineorourke.com/ostomyprograms • 978-281-6126
Are you struggling to live a fulfilling life with your ostomy? Elaine O’Rourke, creator of the “Surviving to Thriving: Overcoming Ostomy Challenges Program, has had an ostomy since 2005 and understands the struggles are real! Stop by to claim your gift, 3 Simple Ways to Eliminate Fears About Your Ostomy.
Takeda
www.takeda.com • 877-825-3327
Takeda is a global, values-based, R&D-driven biopharmaceutical leader headquartered in Japan, committed to bringing Better Health and a Brighter Future to patients by translating science into highly-innovative medicines. Takeda focuses its R&D efforts on four therapeutic areas: Oncology, Gastroenterology (GI), Neuroscience and Rare Diseases. We also make targeted R&D investments in Plasma-Derived Therapies and Vaccines.
Trio Ostomy Care USA
www.trioostomycare.us • 863-421-9400
Trio Ostomy USA, has an over-riding commitment to patient care with improvements to quality of life being at the heart of our business. We ensure that our products reach healthcare providers at an affordable level, offering the benefits of the most advanced silicone technology for all.
United Ostomy Associations of America (UOAA) Inc.
www.ostomy.org • 800-826-0826
United Ostomy Associations of America provides educational material, resources, support and advocacy for those who have or will have ostomy surgery, their family, caregivers and medical professionals. Stop by our booth to view our resources and show your support of the Ostomy and Continent Diversion Patient Bill of Rights by signing the online petition.
Youth Rally
www.youthrally.org • info@youthrally.org
More than 30 years after inception, the Youth Rally continues to provide an environment for young people to meet others who live with conditions of the bowel and bladder. Lasting friendships are formed, in a short 5 nights, in an atmosphere that promotes self-confidence and independence.
Click Here to learn more and register for UOAA’s 7th National Conference Aug. 6-10, 2019 in Philadelphia, PA.