Expect More – Take Control of Your Health Care
Part 2 in Series
By Joanna Burgess-Stocks, BSN, RN, CWOCN, UOAA Advocacy Chair
Good communication skills are the key to problem-solving. This became clear to me when, as an ostomy nurse, I found myself having to unravel what people were trying to tell me when facing a problem. I realized I was speaking a medical language that was not always understood, and my patients were trying to work with that language the best that they could, but miscommunication often happened, resulting in unresolved problems. One day it dawned on me that I needed to do a better job in teaching my patients ostomy language. Sometimes a change just takes a moment of truth.
My moment of truth!
I was excited and determined as a new ostomy nurse to make a difference in people’s lives and knew that I could, after having lived with an ostomy most of my life; since age three. My responsibilities in the hospital setting were to teach people how to care for their ostomy after surgery. I would make sure my patient or their caregiver knew the basics of ostomy care. On the last day before discharge home, I would focus on how to order supplies. I would then say my goodbyes with a simple “call me if you need me”. I realize now, as an experienced nurse, that this was only part of the story. It was not until I became involved with my local UOAA Affiliated Support Group (ASG) and started following online support groups that I became aware of the challenges people experience once they are home and face ostomy care on their own. My moment of truth came one day as I was lying on my bed with my laptop reading story after story on the online support group Inspire of people and their loved ones trying to problem solve skin and stoma issues and difficulties with trying to keep a pouch in place. There I was, an ostomate and nurse who had every resource available to me yet all I could do was offer words of encouragement and some basic information. I realized that I could not adequately offer advice because it was very hard for people to describe what was happening and I didn’t always understand what they were describing to me and sometimes they did not understand what I was saying to them.
Changing my Approach
I started to pay closer attention to what my own patients would say to me when they called with a problem and realized that they too had difficulty describing the issues. I had taken for granted that ostomy medical language was second nature to me, but not for them.
Because the patients were not able to tell me the problems they had with managing their ostomies in a way that I could use, I was often left with more questions. I could only offer limited answers and my efforts to help often felt useless. Being a medical professional for most of my life, I felt humbled realizing that medical language can be difficult for people to understand. Unless you have worked in or been around hospitals, you might not have learned medical words. It is mind-boggling just to know the words to use for ostomies. To get the true feeling, it would be as if I were suddenly thrown into having to build my own house and had to understand all the words involved with building. I would be lost!
The challenges that ostomates face at home motivated me to start an outpatient ostomy clinic connected with my hospital so that my community of people had somewhere to go for help. After seeing patients in the clinic I learned that many ostomates had no idea how to describe the problems they were having with their stoma or skin. Some did not know the type of ostomy they had, some could not describe their stoma and most had difficulty describing their skin problems other than using the words: red, painful and hurting.
Gaining Wisdom:
What I have found over the years, is that the better my patients are able to describe the problems they are having with their ostomy, the more I am able to help them come to a successful solution; whereby, they are able to help themselves. These patients also feel more confident to explore different pouch choices on their own because they have the confidence to tell vendors ( ostomy supply companies) their own stoma and skin problems. Thus the right pouching system “match” is more likely to happen, resulting in a positive result and better quality of life. I now know that just as important as teaching someone ostomy care, it is also important to teach the language that is a part of that care.
As you read these tips on ostomy language, be patient with yourself. It takes anywhere from 6-12 months to speak the language of ostomies according to some ostomy nurses!
Know your Ostomy Type (and whether it is permanent or temporary)
Know How to Describe your Stoma:
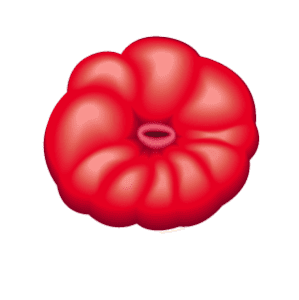
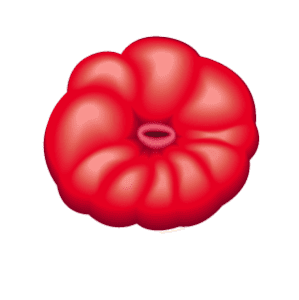
“Stoma” an opening created by ostomy surgery.
It is located on the abdomen and is red/dark pink in color, moist and shiny.
Some describe it as looking like a rosebud.
Take a look at your stoma. In front of a mirror, look at how the stoma changes when you are standing still, twisting from side to side, bending over, sitting, and lying down. Once you have done that, you can ask yourself the following questions about your stoma:
What Does the Skin Around your Stoma Look Like:
- Flat and no wrinkles/creasing
- Skin folds/wrinkles (describe where and when you see wrinkles and folds; for example “ when I sit I have creasing on the right and left side of the stoma”)
Shape:
- Round
- Oval
- Irregular
- Smaller at the top, larger at the bottom
- Larger at the top, smaller at the bottom
- Has one opening
- Has two openings
Color:
- Red
- Pink
- Brown (not normal)
- Black (not normal)
- Maroon, Blue/Purple (not normal)
Stoma Position and Level:
- Below skin level ( in a skin fold or sunken)
- Flush to skin level/at skin level
- Above skin level
Know your Stoma Location:
- Right side of the abdomen above the belly button
- Right side of the abdomen below the belly button
- Left side of the abdomen above the level of the belly button
- Left side of the abdomen below the level of the belly button
- In or near a skin crease
- In or near a skin fold
- On a flat skin surface
Know your Stoma size:
- Use measuring guide to match the size
- Round stomas are measured by diameter
- Oval stomas are measured by widest length and width
- Learn how to measure your stoma here
Know where the stool or urine comes out of the stoma ( this is called the “os” meaning mouth or opening)
- On the top of the stoma and centrally located
- Located on the side of the stoma (left or right)
- Located on the underside of the stoma
- Located level with skin
Know How to Describe your Effluent (output from stoma)
For a stoma that drains feces/stool
- Color: brown, green, black, red and black
- Consistency: thin and watery, loose, thick, soft, formed, pasty
- Odor: no odor, mild odor, offensive
- Amount: High output and loose, High output and thick/formed, no output, low output
- Number of times a day you empty the pouch.
For a stoma that drains urine:
- Color: Clear, cloudy, amber, straw, blood tinged
- Odor: no odor, musty, fishy, fecal ( stool smell)
- Volume: No output, low output, high output
- Substances other than fluid (e.g., grit, crystals, mucus).
Know Your Peristomal Skin ( the skin around the stoma):
- The skin is intact, not raw – no skin breakdown
- The skin has sores – blisters, or looks like a blister without the skin on top
- The skin is discolored (red, pink, purple, bruised)
- Skin sensation (normal, itching, burning, painful)
Normal peristomal skin does not have sores, discoloration, pain, itching or burning.
Final Thoughts on Ostomy “Lingo”
Learning a new language can be difficult. My hope is that you will take the time to understand and know ostomy language so that you too will be an expert. The more you know and understand, the better you will be at expressing your needs and be able to find the best pouching system for you. Use this Know Your Ostomy Checklist the next time you need to talk about your ostomy, and see how much it helps!