By Ellyn Mantell
While walking this morning it occurred to me that for many Ostomates, the heat is very challenging. Ileostomates, in particular, are prone to dehydration because our stoma is always productive. In Mother Nature’s inimitable creation, the colon, or large bowel, is responsible for absorbing fluids and allowing them to be reabsorbed into the body. Since ileostomates either no longer have a colon or it is no longer being used, the precious fluids are flushed from the body through the stoma. Hence the rapid filling and refilling of the pouch, which can be worse in the heat.
Naturally, drinking water is advised. UOAA’s new ostomy nutrition guide recommends you “Make a habit of drinking water throughout the day. At the same time, limit or avoid beverages with added sugars and artificial colors and sweeteners.” Many of us may have difficulty drinking enough to support our anatomy, so we need to be mindful of symptoms that we are lacking the hydration/dehydration balance.
Some symptoms of dehydration include headache, fatigue, dark or decreased urine, lack of concentration, dry mouth, feeling disoriented, shortness of breath, dry skin, stomach cramps. Additionally, leg cramps, loss of appetite, drowsiness, tingling in fingertips and muscle weakness are all concomitant to dehydration.
Learning to live with the chronic dehydration possibility presented to ostomates is certainly attainable. For me, since I do not have a high blood pressure issue which might preclude adding salt, it means adding it frequently at meals. It is strange to servers at restaurants when I ask for the salt shaker, and many have asked if I mean the pepper shaker? We have become a salt-resistant society. But there are those of us who need it for our fluid balance. Additionally, I have a handful of a salty snack before bed, such as pretzels, since nighttime muscle cramps can be very painful and cause sleep deprivation. I keep a bottle of tonic water in the refrigerator, as well as a jar of pickles for those times when nothing else works. For muscle cramps I recommend an over the counter foam moisture. The manufacturers recommend using it prophylactically at night, but I have found it usually very fast-acting when I have foot or leg cramps, so I apply as needed.
Many Ostomates swear by sports drinks like Gatorade, but truthfully, although I have a bottle in the refrigerator at all times in case of fever, I find it difficult to drink. However, if presented with the option of drinking it or winding up in the Emergency Room for fluids, I will imbibe gladly! It’s recommended you dilute sports drinks to reduce the sugar content as well. At some of our Support Group meetings I have heard of many different electrolyte balancing drinks and powders, so you may find one that works for you.
UOAA recommends you drink 8–10, eight-ounce glasses of water/fluid daily. If you have a urostomy this also helps prevent UTIs and keeps urine diluted. Concentrated urine also can cause odor.
View UOAA’s Eating with an Ostomy Guide for more hydration tips such as avoiding excess caffeine, eating foods with a higher water content and sipping your liquids slowly.
It has been recommended that Ostomates drink more than simply water, since it flushes through the system and little gets absorbed before it exits through our pouch. Drink with meals, since food slows down the transport of fluids. Bring fluids with you when you are out and about, since being busy may cause us to forget the responsibility we have to stay hydrated. Lastly, in addition to feeling awful when we are dehydrated, being in that state puts a great deal of pressure on our kidneys, and can lead to kidney failure and lightheadedness, which can lead to falling.
Although this sounds ominous for summer fun, being mindful and smart will help us to relax and enjoy ourselves…after all, with the Covid experience, we have learned to grab the good and be grateful we are as healthy as we are!
Ellyn Mantell is a UOAA advocate and Affiliated Support Group leader from New Jersey. You can follow her personal blog at morethanmyostomy



 I was not in a great deal of pain which was easily managed with Tylenol. I was definitely weak, but otherwise ok. I went home in 4 days, on my own with my urostomy.
I was not in a great deal of pain which was easily managed with Tylenol. I was definitely weak, but otherwise ok. I went home in 4 days, on my own with my urostomy. Rudolph, my red, round stoma
Rudolph, my red, round stoma
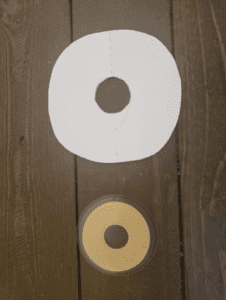
 Night Drainage Pouch
Night Drainage Pouch