Having IBD and/or an ostomy does not prevent a person from getting pregnant and having healthy babies. With the careful supervision of specialists within the fields of gastroenterology, maternal fetal medicine (MFM) and colorectal surgery (CRS), most women with IBD and/or ostomies can have both a healthy pregnancy and a healthy baby.1
With regard to conception, fertility and pregnancy, there are some important considerations to keep in mind:
Conceiving during an IBD flare is generally not advised. If conception occurs during an IBD flare, disease is likely to remain active throughout the pregnancy. Doing so risks poor birth outcomes, including miscarriage, premature delivery, or having a baby with a low birth weight.
It is generally recommended that a person with IBD consider pregnancy when IBD has been in remission for at least 3-6 months and they are not taking steroids. It is not advised that a person become pregnant when starting a new IBD-related medication as it may take time for their body to adjust to the medications.
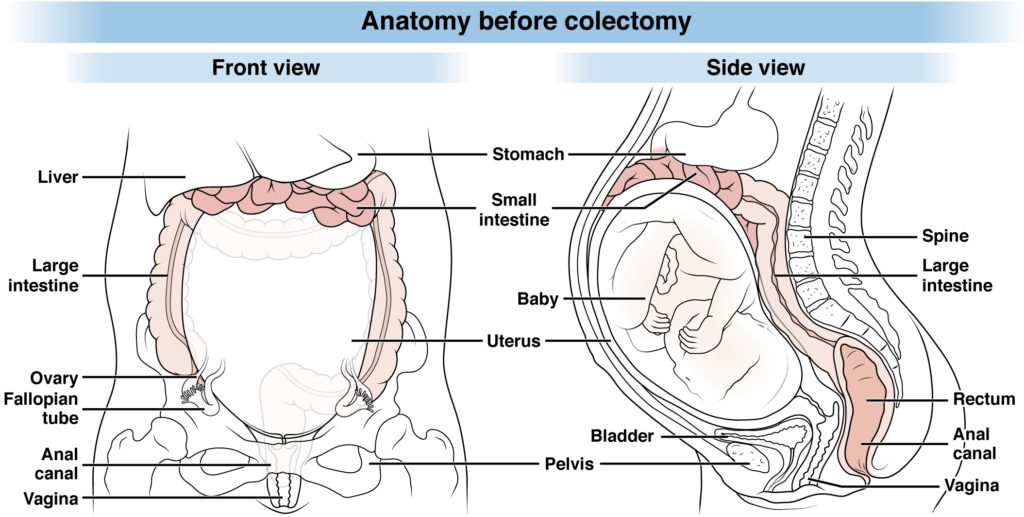
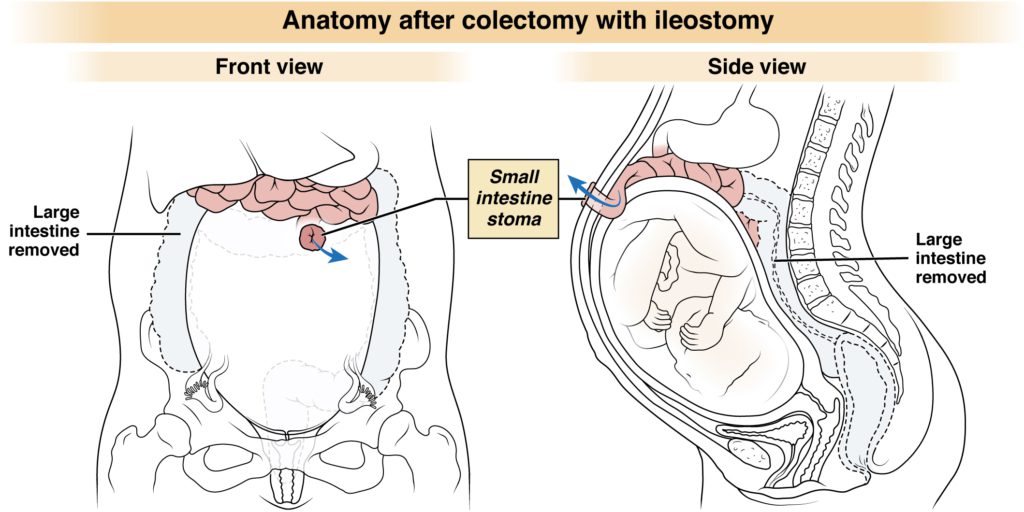
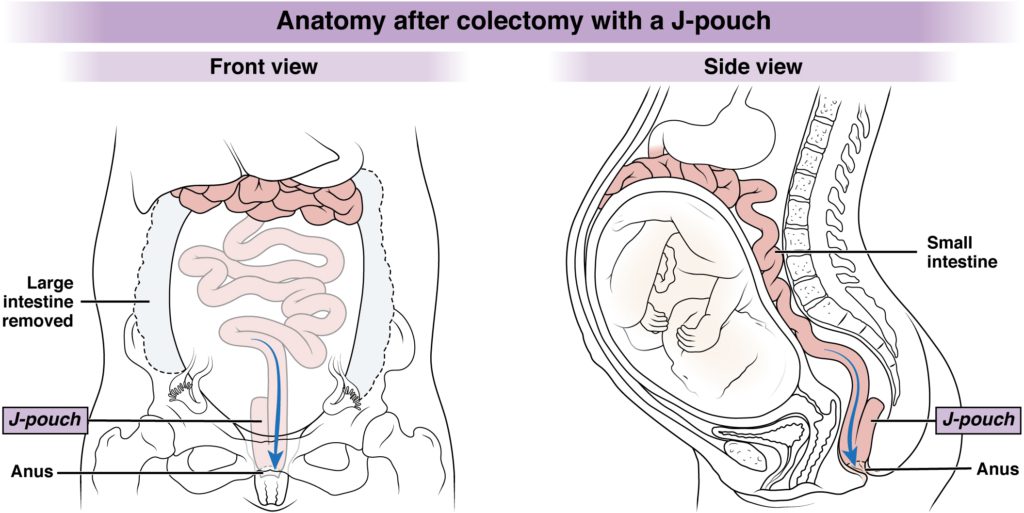
Please refer to the below images to understand what the human anatomy looks like prior to colectomy surgery versus after colectomy with (a) an ileostomy and with (b) a J-pouch/IPAA.
Coordination of Care
The IBD Parenthood Project, an initiative led by the American Gastroenterological Association (AGA), the Crohn’s & Colitis Foundation, the Society for Maternal-Fetal Medicine (SMFM) and Girls With Guts (GWG), lays out in detail how people with IBD should conduct preconception planning leading all the way to labor and delivery. The IBD Parenthood Project outlines how care needs to be well-coordinated amongst healthcare providers and how IBD medications and surgeries affect fertility and pregnancy.
The bottom line is that in order for there to be a healthy newborn baby, the mother should be healthy and in remission. In order to prevent IBD flares during pregnancy, it is important to continue taking prescribed medications as supervised by the mother’s gastroenterologist.2
Pregnant people with IBD should work with a maternal-fetal medicine (MFM) specialist who will coordinate care with their delivery provider, gastroenterologist and colorectal surgeon. An MFM subspecialist should lead pregnancy-related care, and the GI should lead IBD care, with coordinated communication amongst all the providers consulted during pregnancy.
Medications in Pregnancy
In most cases, medication schedules are maintained during pregnancy. However, there are some considerations and exceptions. It is also important to note that if a pregnant person’s IBD status changes, medications or dosages may be altered prior to or during pregnancy.
It is generally recommended to avoid methotrexate, which can cause spontaneous abortion and/or congenital birth defects. Methotrexate should be stopped 3-6 months before conception in both men and women, and should not be taken while pregnant or breastfeeding. Another concern is infertility in men that are on sulfasalazine. Male infertility can be reversed by stopping sulfasalazine well before conception. Many other medications, including biologics and small molecules, should be discussed with your gastroenterologist to ensure how they should be taken, if/when they should be stopped prior to delivery and when they can be resumed again after delivery.
Fertility
While bowel resections do not appear to affect pregnancy in people with Crohn’s disease, people who have had abdominal and pelvic surgery, particularly a total proctocolectomy with an ileostomy or IPAA/J-Pouch, may have lower rates of fertility.3 Men who have had such surgeries may experience retrograde ejaculation and erectile dysfunction, which may affect fertility as well.
Nonetheless, many people with permanent ileostomies or an IPAA/J-Pouch due to IBD have had successful pregnancies by coordinating their care and keeping in close contact with their physicians regarding medication compliance and pregnancy milestones. The same goes for people with Crohn’s disease who have developed fistulae or abscesses around the rectum and vagina.
Written by Tina Aswani Omprakash. Medically reviewed and validated by Jordan Axelrad, MD, MPH. These webpages are funded by a grant from The Leona M. and Harry B. Helmsley Charitable Trust.
- Mahadevan, Uma, et al. (2019). Inflammatory Bowel Disease in Pregnancy Clinical Care Pathway: A Report From the American Gastroenterological Association IBD Parenthood Project Working Group. Gastroenterology, 156:1508–1524. https://doi.org/10.1053/j.gastro.2018.12.022
- IBD Parenthood Project. (2019). American Gastroenterological Association. https://ibdparenthoodproject.gastro.org/
- Isaacs, K.L. (2014) Pregnancy Concerns in Patients with Ileal Pouch Anal Anastomosis for Ulcerative Colitis: Time for Increased Education Across Specialties. Digestive Diseases & Sciences, 59, 1075–1077. https://doi.org/10.1007/s10620-014-3120-8