Part II of a Two-Part Series featuring Emily Rubin MPH, RD, LDN, Thomas Jefferson University Hospital
Earlier this year, I shared the first part of this two-part series on maintaining nutrition and hydration in people living with short bowel syndrome (SBS) and ostomies (e.g., ileostomies or jejunostomies). In Part I, I talked about managing “Output Consistency” – including thickening or thinning out stools, as well as managing stool acidity – with a focus on diet and nutrition. This article addresses hydration considerations, including signs and symptoms of dehydration in people with SBS and rehydration strategies.
Both articles reflect my own clinical experiences, including more than two decades at the Thomas Jefferson University Hospital in Philadelphia where I am the Director of Clinical Nutrition and Lead Clinical Dietitian for the Division of Gastroenterology and Hepatology. These articles are not intended as medical advice. Please contact your doctor if you are experiencing high output, symptoms of dehydration or any other health-related concerns.
As I mentioned in the first part of this series, SBS is a serious and chronic malabsorption disorder that occurs when parts of the intestine are removed surgically or due to injury. The remaining intestine may not be able to absorb enough nutrients from food and drink. When this happens, people with SBS may be at increased risk of malnutrition, dehydration, electrolyte disturbances and/or diarrhea (increased output). I believe that patient education is critical and I am dedicated to teaching my SBS patients about what to expect in terms of stool/ostomy output, along with the risks and symptoms of dehydration. I am proud to share my clinical experience in this article.
| Click here to learn more about SBS. |
MANAGING HYDRATION AND RECOGNIZING THE SIGNS OF DEHYDRATION
A 60-year-old male patient with an ileostomy and approximately 80 cm of remaining small intestine was experiencing increased stoma output (about 2.5 L/day), resulting in frequent watery stools. He reported, “When I drink large amounts of water, I feel fatigued, dizzy, and I have muscle cramps!”
Contributing Factors:
- Experiencing High-Output Stoma: During my consultation with the patient, I explained that excess fluid loss from his stoma led to depletion of electrolytes (sodium, potassium, magnesium), which can cause some of the symptoms that he reported.
- Drinking Hypotonic Fluids: I shared with the patient that drinking hypotonic fluids, including plain water, can actually worsen dehydration by increasing ostomy outputs and making fluid and electrolyte disturbances worse. Hypotonic fluids are less concentrated than that of the fluids in the body. In addition to water, these types of fluids include plain, unsweetened tea, black coffee and sugar-free sodas.
- Diet Low in Complex Carbohydrates: When the patient said that he consumes simple sugars and high-fat foods, I told him that these food choices draw excess water into the bowel, increasing stool output and worsening dehydration. Concentrated sweets, such as candy, cookies and cakes, as well as sweetened beverages like soda, juice and lemonade are all examples of simple sugars.
Understanding Stoma Output Levels
For people living with an ostomy, including those with SBS, I believe that understanding normal output levels is important for managing health. Typically, an ileostomy (post-op) produces around ~750mL per day, although output can be 1200mL or more per day initially. A jejunostomy, on the other hand, can produce significantly more—up to 6 liters per day. In contrast, a colostomy produces between 200-600mL daily. I tell my patients that it is important for the body to make at least 1000-1200mL of urine each day to protect the kidneys.
A high-output stoma occurs when output exceeds ~2 liters per day. This can lead to dehydration and the loss of essential minerals like sodium and magnesium, which are critical for overall health. For people with SBS, high stool output can significantly increase the risk of sodium depletion, with potential losses reaching up to 2430 mg per liter of output. I tell my patients who are experiencing high stool output and symptoms of low sodium, such as unexplained weight loss and fatigue, to contact their doctor.
Restricting Intake of Hypotonic Fluids
When I see patients with SBS who are experiencing high-output stoma in my clinical practice, I advise them to restrict the intake of hypotonic fluids like water, tea, black coffee, and sugar-free sodas. These fluids pull sodium (salt) into the small bowel, and bring water along with it, leading to increased stool outputs. In people with SBS, this can exacerbate fluid and electrolyte imbalances due to the lack of absorptive surface area for both salt and water in the remaining bowel. Drinking more water can worsen the condition by creating a cycle of increased ostomy outputs, associated dehydration and thirst for more water. Continue reading for rehydration options included in this article.
Dietary Factors Contributing to Dehydration
Foods that are low in complex carbohydrates and high in sugar can draw water into the gastrointestinal tract. These, too, can worsen stool output and cause fluid and nutrient losses for people with SBS. I have seen firsthand in my patients that choosing complex carbohydrates, like white rice, potatoes, pasta, bread and bananas can help manage stoma output and improve nutrient absorption. These carbohydrates are easier to digest and absorb compared to simple sugars.
RECOGNIZING THE SIGNS OF DEHYDRATION
Did you know there are relatively easy ways to track hydration levels?
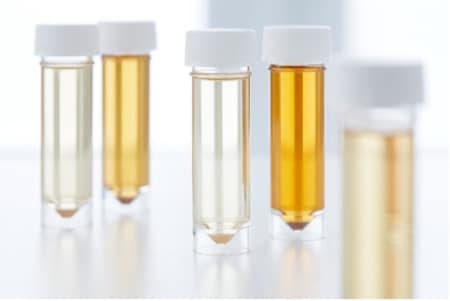
Urine Color
I tell my patients that monitoring their urine color can be a relatively easy yet effective way to keep tabs on their hydration levels. If the urine is darker than a pale yellow, it might suggest that the body is holding onto water rather than getting rid of it properly. Clear or light, yellow-colored urine reflects hydration. Darker shades of urine could signify dehydration.
Other signs of dehydration include:
- Rapid weight loss
- Higher stool output than total fluid intake
- Less-frequent urination
- Fatigue
- Lightheadedness/Dizziness when standing
- Dry mouth
- Thirst
I tell my patients to consult their doctor if stool output increases, urine output decreases and they notice signs of dehydration.
Water-Tracking Apps
I have encouraged many of my SBS patients to set hydration reminders or alarms on their mobile phones. I have also suggested trying out water-tracking applications (or “Apps”). There are some water-tracking Apps that offer gentle hydration-related nudges throughout the day. Some Apps can help set goals and hydration-tracking progress. There’s even an App that lets users grow a virtual plant by staying hydrated! Searching for “water tracker” in an “App” store on your mobile device, tablet or desktop computer should bring up several options.
REHYDRATION
Did you know that Oral Rehydration Solutions are different than Sports Drinks?
Oral Rehydration Solutions (ORS)
When my patients with SBS are experiencing high output stomas leading to dehydration, I often try to incorporate Oral Rehydration Solutions (ORS) into their rehydration plans. ORS have a specific combination of sodium, carbohydrate and water in a special ratio that can enhance fluid absorption across the small bowel wall, even when the patient is experiencing diarrhea. In many of my SBS patients, I’ve seen this tailored blend help the body absorb those electrolytes like a sponge. However, ORS can be difficult for some people, because of the salty taste. Sometimes people find it helpful to make ORS into ice cubes or popsicles. Sugar-free flavoring can also be added to help improve the taste of the ORS.

Patients have asked me why they can’t simply buy Sports Drinks – such as basic electrolyte drinks – to rehydrate themselves. While Sports Drinks do contain electrolytes like sodium and potassium, as well as sugar, they are not ideal for SBS patients for effective rehydration. For example, they often have too much sugar and not enough salt. It is the special ratio of sodium, carbohydrate and water that can help with fluid absorption across the small bowel wall.
| You can make your own ORS at home. Download a free-of-charge ORS recipe book here:
https://shortbowelsyndrome.com/Content/pdf/Recipe_Book_DIGITAL.pdf |
If you are living with or caring for someone with SBS, I hope that the information that I have shared in this two-part article series helps empower you to bring questions about nutrition and hydration to your healthcare team. Consistent communication is critically important, and I encourage you to bring any concerns to your doctor, nutritionist, dietitian or another member of your SBS healthcare team.
Sometimes it can be challenging to find a healthcare provider who treats rare GI conditions like SBS. To check if there is a medical provider with SBS experience in your local area, visit https://shortbowelsyndrome.com/find-a-provider.
+++

Emily Rubin MPH, RD, LDN is the Director of Clinical Dietetics, Clinical Dietitian for Division of Gastroenterology and Hepatology at Thomas Jefferson University Hospital in Philadelphia. In addition to her extensive clinical work, her expertise and insights in the areas of diet and nutrition have been featured in numerous online and broadcast media outlets.
This article was created by Takeda.
Editor’s Note: This educational article is from one of our digital sponsors, Takeda. Sponsor support along with donations from our readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.
US-NON-11817v1.0 03/25















 If you must travel during this time, make sure you pack
If you must travel during this time, make sure you pack  The holidays can be emotionally challenging for everyone, but for those dealing with chronic conditions, things may feel a little tougher. If you are feeling blue, that is ok! All emotions are valid, so give yourself the time and space to feel sad or angry and to grieve what was. But it’s also a great time of year to reflect on the things that you are grateful for, whether that’s your support system, your health, or even just for making it through this crazy year.
The holidays can be emotionally challenging for everyone, but for those dealing with chronic conditions, things may feel a little tougher. If you are feeling blue, that is ok! All emotions are valid, so give yourself the time and space to feel sad or angry and to grieve what was. But it’s also a great time of year to reflect on the things that you are grateful for, whether that’s your support system, your health, or even just for making it through this crazy year.


