Subject of the movie White Boy Rick reveals why depicting his ostomy was critical to the story.
By R.S. Elvey
Hollywood movies, both fictional and nonfictional, thrive on melodramas depicting romance and violence. Car crashes, explosions, shootings, and all kinds of mayhem deliver gruesome injuries to victims and survivors. The 2018 film White Boy Rick, starring Matthew McConaughey and Richie Merritt, has all these components but is unique in showing the personal aftermath of a violent act – in this case scenes depicting an ostomy.
The film, set in the 1980s on Detroit’s eastside, tells the true story of Rick Wershe, Jr., called by the local newspapers “White Boy Rick” and his father Richard Wershe, Sr. During that decade, Ronald Reagan’s War on Drugs is in full swing and the FBI is anxious to break up drug dealing and crooked police in Detroit. Agents observe 14-year-old Rick mingling with a local drug lord and his father selling illegal guns to drug gangs. They meet with Rick and his father and offer them a deal. To prevent his father from going to jail, Rick, at 14, would become an informant working for the FBI. His father agrees to the deal and Rick becomes the youngest informant ever undercover for the FBI.
While working for the FBI, Rick becomes more and more involved in the daily activities of a leading Detroit drug lord and his gang. They become suspicious of Rick and he is shot in the stomach by a .357 magnum. The bullet enters and goes clean through, severely damaging his large intestine. He is rushed to Ascension St. John’s Hospital, Detroit, where lead surgeon Dr. Norman Bolz and others save his life. He awakes with a lifesaving ostomy.
The first time the ostomy pouch appears in the film is when Rick and his father are coming home from the hospital. Rick has his left hand over his stomach and the pouch is overlapping his pants. He is also depicted emptying his pouch. In a recent correspondence with Rick from prison he said, “When I woke up, I didn’t realize that I had it. I think I touched my stomach and then first felt the bag. I didn’t know what the bag was. Dr. Bolz came in and explained to me what the bag was and how it worked. The bullet had torn through my intestines and the doctors were hoping the intestines would heal and that it could be reversed, but that it would take a while.”

Rick Wershe, Jr. “White Boy Rick” when he was convicted in the 1980’s and today behind bars over 30 years later.
Top photo credit: Sony Pictures
While in the hospital the staff showed him how to empty and change his pouch. At home he was never seen by an ostomy nurse or received any other ostomy maintenance training. He said, “I basically had to learn on my own. Fortunately, I really didn’t have any skin problems. I had to keep the bag clean and was able to do a pretty good job. I had skin irritations but it was not too bad. I was lucky.” His friends were young and they were shocked when they saw his bag. But he said, “My family, especially my dad and grandparents, tried to be as helpful and supportive as they could.” He also met others who had ostomies. Rick had to pay for his own supplies at a local pharmacy which proved very expensive. His father wanted him to wash and reuse the pouches but Rick wouldn’t do that. He would use 2-3 new pouches a day.
Andy Weiss, one of the movie’s screenwriters, spoke numerous times with Rick while working on the screenplay. When asked why the ostomy scenes were included he said, “The ostomy scenes are the core of showing Rick’s vulnerability and what I was hoping to get from it was the sympathy and empathy that he deserved but never received from law enforcement or the people around him at that time.” Rick insisted that his ostomy should be part of the movie saying, “We included the ostomy scenes because I thought it was important to show young kids and adults that you can go through this and still be ok.” And get through it he did. Rick says that the ostomy proved to be no hindrance either socially or in his daily dealings. A year and a half after his original surgery, Dr. Bolz performed a successful revision.
Rick soon faced even greater challenges. Abandoned by the FBI and his family needing money, Rick and his father turned to the only way they knew how to make money, dealing drugs. Eventually, Rick was arrested and sentenced to 30 years for drug dealing. Now 49-years-old, he is scheduled to be paroled in 2020.
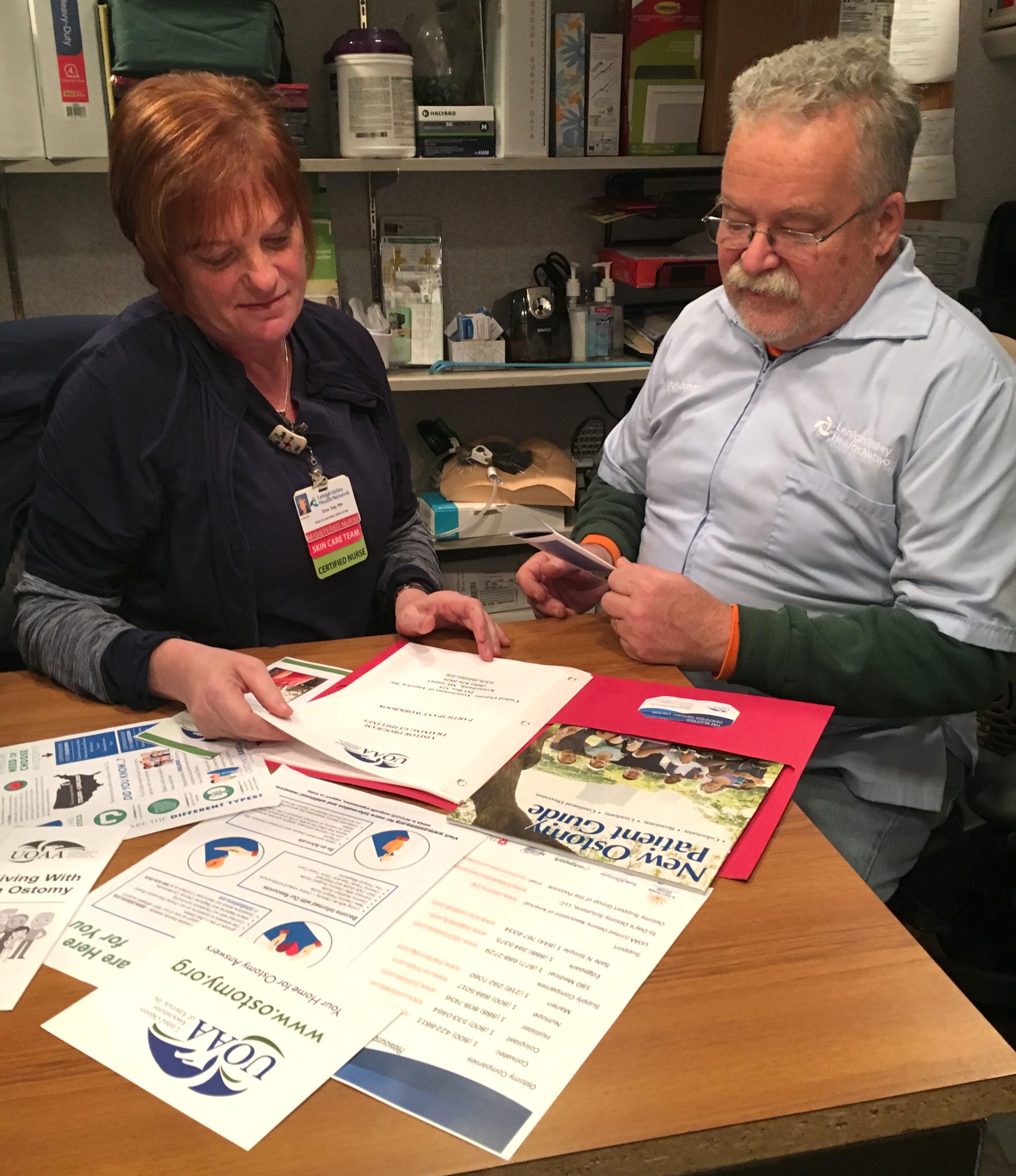
When ostomates watch the movie, the ostomy is immediately recognizable. But numerous reviewers of the movie never mention the ostomy scene. Ostomate, Robin Glover on ostomyconnection.com, wrote after viewing the film, “There were some inaccuracies, but it will definitely raise awareness and change what the word “ostomy” conjures up in the mind of anyone that sees it.” Joy Hooper, United Ostomy Associations of America’s 2019 WOCN of the Year was enthusiastic in her response to the film and said of the screenwriter, “I appreciate his way of displaying life with an ostomy. He did a superb job. He was able to show what many consider a negative aspect of life respectfully.”
White Boy Rick is now available on streaming services.







 I was told if I didn’t have the surgery when I did, my Crohn’s disease would have killed me. Surgery made a drastic change in my life for the better. Now I will be around for my wife and kids.
I was told if I didn’t have the surgery when I did, my Crohn’s disease would have killed me. Surgery made a drastic change in my life for the better. Now I will be around for my wife and kids.

