Expect More – Take Control of Your Health Care
Part 5 in Series
By Jeanine Gleba, UOAA Advocacy Manager and Sue Mueller, CWOCN
In Part 5 of the Expect More – Take Control of your Health Care series, we tackle the sticky subject of health insurance and the importance of knowing what you’re getting in your policy. How many people plan on getting an ostomy? It’s one of those things that happens in life. So you learn to live with it and then adding insult to injury you discover that the health care insurance you had proves to be inadequate to cover the costs of your ostomy supplies. You are stunned to discover that ostomy supplies cost $300-$600 a month. Suddenly you’re expected to adjust to your new circumstance and also cope with a significant cost as you scramble to find solutions.
Every year individuals have an opportunity to re-evaluate their health care needs and insurance coverage, and if need be, during that window of opportunity, change health care plans or increase coverage.
How do YOU get your health care insurance?
First step is to know exactly where your coverage is coming from so you know where to get information from and ask questions.
You get health care insurance:
- Through your employer (usually you and your employer share costs)
- When you buy your own healthcare insurance from your state Health Insurance Marketplace
- You qualify for Medicare by age and work history
- You qualify for Medicare by disability and work history.
- You qualify for Medicaid because you are a dependent child,are a parent of a dependent child, or by low income.
- You qualify for military health benefits because you or your family are active US military, or have retiree benefits.
- You qualify for veterans benefits because of your military service and honorable discharge.
- You qualify for American Indian/Alaska Native healthcare coverage.
What are your medical needs?
You can begin to determine your needs by calculating your medical risks. What is your medical history and your family’s medical history? What are your lifestyle health behaviors (i.e., diet, exercise, smoker etc.)? As you age, your medical risks increase, so take this into consideration when planning health insurance coverage. If you have several medical diagnoses/pre-existing conditions (e.g.., colostomy, urostomy or ileostomy), take prescription medications, and require visits with specialist physicians you have different needs and risks than someone with no diagnoses and no prescriptions.
So what is the best employment and financial strategy for you? If you can’t afford marketplace healthcare insurance can you or your spouse become employed by a large company with comprehensive benefits? What is your age? You might make one choice at your present age and another choice at a later date. Ask around, educate yourself, every state has a number to call to get healthcare insurance information (ask for SHIP- state health insurance assistance plan). For example, some people don’t understand that they need to sign up for Medicare Part B insurance (where ostomy supplies are covered) when they are first eligible or simply don’t because of the additional premium due. Others have been misinformed and thought the VA would cover all their healthcare needs; however, they actually need to sign up for Medicare A and B AND use the VA. Also many people don’t realize that there is a penalty for not signing up for Medicare B and D when you are first eligible.
Once you calculate your medical risks, examine your finances and are choosing a healthcare policy, you need to know:
Your health insurance policy is an agreement between you and your insurance company, a contract. The policy lists a package of medical benefits such as tests, drugs, and treatment services. The insurance company agrees to cover the cost of certain benefits which are listed in your policy. These are called “covered services.” Your policy also lists the kinds of services that are not covered by your insurance company, and circumstances that are not covered (exclusions). You have to pay for any uncovered medical care that you receive. Don’t confuse what your policy covers with what is “right”, what your neighbor’s policy covers or what you think you are “entitled to”. What is covered is what is stated in your policy. If you understand this key concept it will save you a lot of stress down the road. This concept is true for Medicare, for Medicaid and all other health insurances who set the terms (rules) of the insurance policy agreement that you have made with them.
Insurance Basics
Some other items you need to know about your health insurance are these basic terms:
Plan Types- HMO (Health Maintenance Organization, managed care), PPO (Preferred Provider Organization ), POS (Point of Service). They all have different rules.
Premium- If you have employer sponsored insurance this is the amount you or your employer pays for your insurance coverage. Frequently you pay part and your employer pays part. If you are buying the insurance independently this is what you pay for your insurance. This is paid even if you don’t need to go to the doctor or use your insurance. Insurance costs vary by state.
Deductible- What you need to pay before your insurance kicks in. (Original Medicare and many companies have an annual deductible which must be met. Some people save money on the cost of insurance premiums by buying high deductible policies). You may get denied for supplies or a service because you have not met your deductible for the year. For example, someone with an annual deductible of $4,000 will have to pay for all of their supplies or health services until they reach that $4,000.
Coinsurance- The percent of the cost that you are responsible to pay for covered services after you meet your deductible. (ex. Original Medicare pays 80% of the Medicare approved amount of a covered service you pay 20% unless you have a supplemental policy which picks up the remaining 20%). Medicare Advantage Plans/Type C insurances set the costs of the copays which are covered in their benefit booklets. Some people have purchased insurance through the Affordable Care Act (Obamacare) Marketplace and tried to save money on premiums but found that they are responsible for 30% of the costs with insurance paying 70%.
Copay- This is the fixed amount of money you pay for certain services such as prescriptions or MD visits. Usually, visits at urgent care or the emergency department have higher copays. These rules are all listed in your insurance policy and/or benefits book. For example, a plan might indicate that you pay $20 for each doctor visit.
In-Network versus Out-of-Network Benefits- An in-network provider is one contracted with the health insurance company to provide services to plan members for specific pre-negotiated rates. Typically, when you see an in-network provider you receive 100% coverage. An out-of-network provider is one not contracted with the health insurance plan and you will need to pay a percentage of the cost of the services (usually insurance covers 80% and you pay 20%).
Accepts Medicare assignment- Means your doctor, provider or supplier agrees to accept the Medicare-approved amount as full payment for covered services.
Non participating providers have NOT signed an agreement to accept an assignment. They can charge you more than the Medicare approved amount up to the “limiting charge”.
Maximum Out of Pocket Expense- This is the maximum amount that you pay for in-network services and prescriptions in a calendar year. This includes the deductible, coinsurance and copays. It is wise to keep track of what you have paid for and be aware of the amount of the maximum because after this amount is reached the services are covered 100%.
For a more complete list of insurance term definitions visit this website.
All of the above can change, so it’s important to annually review your plan and see if it still meets your needs. This can greatly affect the cost to you for your health care, so it’s always a good idea to compare plan options, estimate the costs of your care and consider all of the insurance costs (premium, deductible etc.). How well does your insurance cover your needs? For example how much do your supplies cost each month and how much will you pay out of pocket until your plan coverage starts paying the bill? UOAA gets many calls from people who are looking for help with paying for their ostomy supplies because they can’t afford their high deductibles or copays.
Are your ostomy medical necessities a covered benefit?
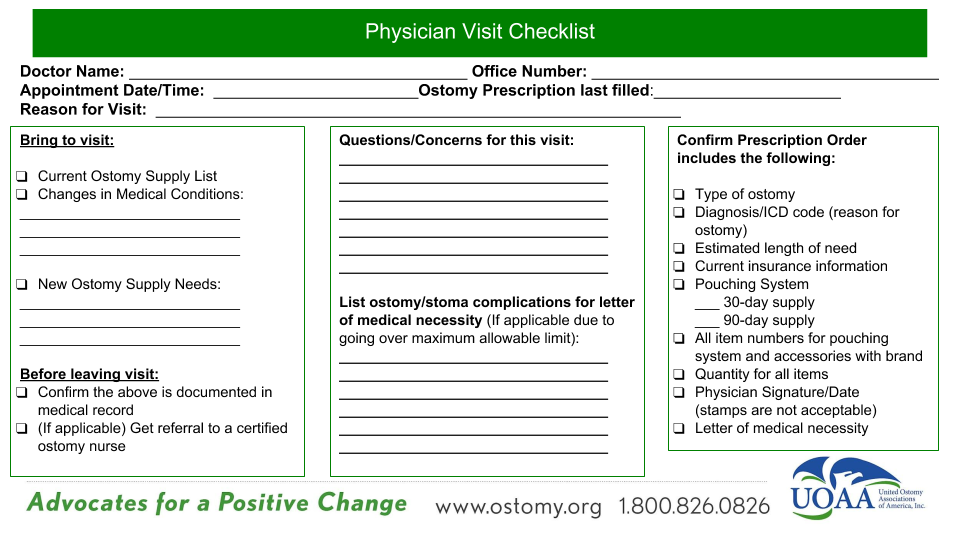
Is a medical necessity the same as a covered benefit? A medical necessity is something that your doctor has decided is necessary. A medical benefit is something that your insurance plan has agreed to cover. In some cases, your doctor might decide that you need medical care that is not covered by your insurance policy. Insurance companies determine what tests, drugs and services they will cover. These choices are based on their understanding of the kinds of medical care that most patients need. Your insurance company’s choices may mean that the test, drug, or service you need isn’t covered by your policy and then you will need to pay for that service or item. It’s important to know what is covered by your insurance policy such as your ostomy supplies, so you will need to consult the summary plan description and evidence of coverage, (ex. benefits booklet, Medicare and You publication). The customer service agent may be able to tell you how to document your need or what they require if you have a medical reason to need more or different supplies.
Knowing what you need and being able to explain it is vitally important. Don’t expect people who don’t have an ostomy or experience with an ostomy to understand what you need. An example of this is the gentleman who had a new ostomy and went to an insurance broker to choose a Medicare C /Medicare Advantage Plan. He was assured that the plan he chose was an excellent plan and certainly covered all the bases. What resulted was that he had very high copays for his supplies and it was not a good plan for him at all. He also was not aware that if you join a Medicare Advantage Plan for the first time and you aren’t happy with the plan, you have special rights under federal law to buy a Medigap policy if you return to Original Medicare within 12 months of joining (Medicare and You- section 5).
Today the vast majority of health insurance plans do cover ostomy supplies, but how they are covered varies. Make sure you ask if the plan will cover what you need and how they will cover it. As you compare plan options and shop around ask yourself these 10 Questions to Ask Before You Choose a Health Plan.
Final thoughts
It is critical that as an ostomate you be your own patient advocate and ensure your health plan covers your medically necessary ostomy supplies. Insurers should not determine your medical treatment plan. That should be between you and your medical professional.
Really, there is a logical structure, rhyme and reason to all this health insurance business and if you approach it with that in mind you will be more successful. For more information on insurance reimbursement check out this webinar.
Take the time and effort to do some necessary research on insurance plans to find the best quality, and most cost-effective to meet your ostomy needs and financial situation. In the long run you’ll be thankful you did.
Take control of your healthcare and don’t let your health plan let you down!
Disclaimer: UOAA does not provide insurance advice or financial assistance for supplies. We do recognize there may be times for emergency supplies. Please use this list of resources which may provide assistance on a temporary basis.