Tag Archive for: ostomy bag
By Ellyn Mantell
Welcome to my fantasy.
We all have our fantasies, so come along with me as I describe one of mine…new ostomates (those with ileostomy, colostomy or urostomy, all having had stoma surgery) would begin their adjustment to their new life with all of their questions answered, they would have knowledge and be welcomed into an Ostomy Support Group, they would have a connection with a Wound, Ostomy, and Continence Nurse (WOCN) and they would recognize what a gift, what a lifesaver an ostomy is.
My concern is that this is not the usual for ostomates, either new or even those who have them for many years. In New Jersey, particularly where I live, there are many resources available, and yet, even in our sophisticated arena, many ostomates leave the hospital uninformed and underserved. Prior to Covid-19, I visited patients in the hospital or in rehab facilities to answer their questions. I brought journals and pens so they could write their emotions, concerns, and observations, and refer back to their notes as they made progress. I am so anxious to return to that important undertaking as soon as it is safe to do so.
When I had my surgery in March of 2014, my surgeon told me I would be in the hospital for 5-7 days. However, I felt so well, so quickly, that I was able to leave 4 days later. That was pushing the envelope, but I was so used to recovering from abdominal surgeries, having had 22 before that, my ability to go into recovery mode was well-entrenched. The majority of patients need so much more time, and now, even 4 days is more than they are offered.
Back to my fantasy, and my pipe dream of a great transition for new ostomates:
How can questions be answered, and knowledge gained as needed?
The majority of ostomies, even those performed in an emergent situation, require marking the abdomen for placement of the stoma (opening.) That is typically done by the Wound, Ostomy, and Continence Nurse (WOCN) and that is the person who comes to the patient’s room post-op to begin to prepare the ostomate for life at home. In an ideal world, the WOC nurse has written information to share, which once home, will make more sense, and provides contact information for any questions. Additionally, the ostomate is put in touch with the United Ostomy Associations of America to become part of a bigger group of kindred people.
How do we find Ostomy Support Groups in our area?
I am involved in three Support Groups, becoming president of one already formed when I had my ileostomy, and then worked with WOC nurses at two other hospitals in the area to form new ones. Until Covid hit, these were growing so nicely. But we are meeting virtually now, and staying as close as possible, knowing that the day will come when we are back together. It is wonderful to see “my people” who share my concerns, experiences and fears and accomplishments. We help each other in countless ways. People reach out to me through the WOC nurses in the area, United Ostomy Associations of America, The Phoenix Magazine, the American Cancer Society, three hospitals, and through word of mouth. Because I am so open and revealing about my ileostomy and Lily, my stoma, I believe my name pops into the minds of people when they know someone in need.
Ostomies are Lifesavers! “Read all about it!”
An ostomy provides the gift of health for many, many medical situations, including cancer, ulcerative colitis, Crohn’s disease, diverticulitis, motility issues and devastating organ injury. We live in good times for our supplies and the ability to try new and innovative appliances and accessories. The Phoenix Magazine is a great resource for all, and assists in wading through the confusion many feel. Motivational stories and practical guidance round out the offerings.
A final word about those we call our Angels…the Wound and Ostomy Nurses.
Establish a relationship with one, and if there is an Ostomy Clinic or Ostomy Center in your area, use it! These nurses are your connection to properly-fitting appliances, the correct supplies and accessories, questions and personal support, as well as the ability to refer to a Support Group. More and more are entering the private sector and providing services such as home visits, particularly to those who cannot travel to a clinic or office, and your surgeon may even have one in the office to help navigate the transition to life as an ostomate. We call our WOC nurses our Angels, and that is exactly what they are, ladies and gentlemen with big wings to support us!
Ellyn Mantell is a UOAA advocate and Affiliated Support Group leader from New Jersey. You can follow her personal blog at morethanmyostomy
A convex ostomy skin barrier can help prevent output leakage and skin issues. Unfortunately, some misconceptions about convexity may keep people with ostomies from using it.
A convex pouching system refers to the shape of the back of the ostomy skin barrier – the side that goes against your skin. A convex skin barrier is not flat, rather it is curved or dome shaped. Using an integrated convex skin barrier is often referred to as “adding convexity” to a pouching system. This convexity provides a gentle push on the belly, allowing the stoma to protrude up and outward. This can help output go directly into the pouch and not under the skin barrier (which can cause a leak).
Common reasons for using convexity are to prevent leakage and related skin issues, and to avoid having to change the pouching system more frequently. If your pouching routine or body weight has changed, chances are it’s time to consider using a convex skin barrier.

Flat Skin Barrier

Convex Skin Barrier
Below are a few myths or misconceptions about using convexity:
- All convexity is the same
Convexity should be chosen and customized based on your specific stoma and body shape. There are two main types of convexity: soft and firm. Soft convexity is flexible and conforms to your body as you move. Firm convexity is rigid and provides firm support around your stoma to help it stick out. In most cases, soft convex skin barriers are used on firmer abdomens, and firm convex skin barriers work best on softer abdomens. Someone may have a bad experience with convexity, only to learn that it was the wrong type for their stoma, body shape, or output. It’s important to know that the convex skin barrier opening needs to be close to the stoma in order to help the stoma protrude. This will also help reduce the possibility of leakage.
- A convex skin barrier is uncomfortable or even painful
If your convex skin barrier is causing pain or discomfort, you are not wearing the right type of convexity. Based on your needs, and with guidance from a healthcare professional, consider trying some of the many convex barrier options available and see if they make a difference. The importance of addressing leakage should outweigh the fear of trying something different. Use the health of the skin around your stoma as a barometer. If your skin looks good, and you are not leaking, you’ll know you’re using the right type of ostomy skin barrier for a good fit.
- I have to wait to use convexity
You don’t need to wait a certain amount of time before using a convex skin barrier. Each person is different. Some may need to add convexity immediately after surgery, while others may not need to add it at all. There is no concrete rule, and it depends on the type of stoma you have and how well it protrudes. If your belly is soft enough, you can start right away. Again, it’s important to prevent leakage while keeping the skin around your stoma healthy, and trying convexity could help accomplish both goals.
- If my stoma is level with my skin, I need a convex skin barrier
In most cases this is true, but choosing a type of convexity can depend on your stoma output. There are always exceptions and everyone has different experiences. For example, someone who has a colostomy with formed stool and regular bowel habits may not need to use convexity, even if their stoma is flush to the skin. That’s because formed stool is unlikely to leak underneath the skin barrier. On the other hand, more liquid output can increase the chances of leakage.
Consider trying a convex ostomy skin barrier to see if it will help prevent leakage and skin issues, and increase your pouching system wear time (i.e., how long you can wear your skin barrier before it fails). Convex skin barriers come in both pre-cut and cut-to-fit options and are covered by most insurance plans. An ostomy nurse can help determine which type of convexity is right for you and when you should use it.
For more information on skin barrier convexity and other resources, visit the Hollister Ostomy Learning Center.
Terri Cobb earned her RN degree in 1991 and became a board-certified CWOCN in 2011. Currently on staff at the Cleveland Clinic in Cleveland, Ohio, her responsibilities include caring for ostomy patients of all age groups from the neonate and beyond. Terri interacts with patients in all phases of their journey from pre-op, to immediate post-op and through follow-up care. Financial Disclosure: Terri received compensation from Hollister Incorporated for her contributions to this article.
Editor’s note: This article is from one of our digital sponsors, Hollister Incorporated. Sponsor support along with donations from readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.
Ostomy Nurse Anita joins host Elaine O’Rourke (an ostomate and IBD patient) to discuss the different challenges that ostomates (ileostomy, colostomy) face with output. Learn what you can do about pancaking, high output, different consistencies, bag ballooning up, ostomy pouch options, filters or no filters, open and closed-end pouches and much more.
A good dose of humor is included! Nurse Anita, RN CWOCN offers private consultation: www.anitanurse.com.
Elaine works directly with people with Ostomies, Crohn’s Disease, Ulcerative Colitis. If you are struggling please reach out to her. Grab the free guide via www.ElaineOrourke.com (under IBD or Ostomy programs) “3 simple ways to eliminate fears about your ostomy” or “Hidden Causes: 5 mistakes even well informed people with IBD make”
My name is Jodi Capobianco, I am 54 years old and have a permanent ileostomy. Five years ago I was diagnosed with severe off-the-charts constipation and was to receive a temporary loop ileostomy.
I am so thankful that I did not let having an ostomy get in the way of me missing out on this awesome adventure.
Shortly after my surgery, I began having problems. To make a long story short, my colon became diseased and they removed it giving me a permanent ileostomy. Unfortunately, shortly after my colon was removed I developed an abscess. I actually ended up developing seven more before an amazing surgeon figured out that I had a leak. He performed a small bowel resection and made my loop ileostomy an end. That was over two years ago. I was so weak when I came home I was using a walker. I can honestly say life is now amazing. In fact, I just got back from rafting the Colorado River in the Grand Canyon for eight days.

There were no bathrooms, heck there was no nothing just the big outdoors. I went with my husband, our trip started on a Saturday morning when we flew from Boston to Arizona. I was pretty pumped when my ostomy was not an issue while going through security. Not that it is a big deal to be patted down, but it was nice to be able to skip it. When I fly I try to limit my intake so I am not having to empty on the plane. I also stay away from anything carbonated when I am out, so no bubbles. We arrived in Arizona after traveling for about 9 hours. We headed to our hotel, where of course our room was not ready and got lunch. I knew I would be near a bathroom for the afternoon and evening so I ate what I wanted.
That night was the orientation for the trip. I learned we would on the bus for about three hours the next morning with no bathroom break. Departure time was 6:45 am. I decided not to eat breakfast but brought a bagel with me. I ate about an hour into the trip. I knew I would be able to use a porta-potty at the boat launch. On the morning of the trip I changed out everything. I ended up using wafers that were precut. I usually cut my own but I did not want to have to deal with that. I used closed-ended bags that were waterproof. I am usually a drainable girl, but again I knew there really would not be a place to drain anything especially during the day. I also used three brava strips for reinforcement, and I use a ring under my wafer.
I had two complete changes in my dry bag, then in my shorts or pants I had three bags in a zipper pocket, I also kept a bag in my backpack in case we went hiking.
We were all given two dry bags for our stuff, one we could get to during the day and one we could not. In my day bag, I had enough supplies to do two complete changes, 5 disposable closed ended bags as well as five bags I could put the disposable bags in. The first night when we stopped at camp I was given my own ammo box. This was a metal box that sealed. I was able to put all my waste into it. In the morning I would give the box to the trip leader, she would empty it and then when we stopped at camp for the night she would discretely give it back to me. The only bathroom in the camps were either behind a tree or rock and they consisted of a yellow bucket with a toilet seat on it to pee in and a metal bucket that contained waste. I would pee in the yellow bucket but luckily did not have to deal with the smelly bucket for pooping in. I would simply pop bags on and off when I needed to.

When we arrived at the camp for the night, which generally was a large sandy area by the side of the river, we all helped unload the boats. Once the boats were unloaded, one would find their campsite for the night, lay out a tarp and sleeping pad. This is when I would take a minute to get organized. For me, this consisted of placing two closed-ended bags and baggies in a plastic cup near my sleeping bag. This was so I could change in the middle of the night if I needed to. I also would place my headlamp nearby so I could find it easily in the dark and see what I was doing.
When popping a pouch on and off, I would place a small baggie (I used the blue ones that came with my bags) under the disposable bag so when I unclicked and popped it off it went right into that bag. Next, I would pop on a new pouch and be good to go. For the most part, I changed bags when we got to camp, right before bed, once in the middle of the night and when I woke up.
Having the precut wafers and closed ended pouches made all the difference in the world.
During the day I would set myself up as follows: I had two complete changes in my dry bag, then in my shorts or pants I had three bags in a zipper pocket, I also kept a bag in my backpack in case we went hiking. I would change bags after breakfast before getting on the boat and when we stopped for lunch. I was generally good until we got back to a camp.
To change I would hide behind a rock or a tree or sit on my sleeping bag with my back to everyone. I also had a small package of biodegradable baby wipes with me.
There were two times I had to change everything. The first was three days into the trip. I got off the boat and my skin itched. This is generally a sign for me that something is leaking. I had been in the water a ton this day so I was not surprised. I peeled off all the adhesive from the brava strips as best I could, dried the area off, and put on a new wafer and popped on another bag. The second time was two days later. I knew that this time I really needed to wash the area and try to get a bit of the adhesive off my skin. So, I went down to the river with a small washcloth that I had packed. I took everything off and dipped the washcloth in the river and then scrubbed my skin as best I could. I dried the area, covered my stoma with the cloth and went back to my campsite where I put on a new ring, wafer, brava strips and pouch. I did this all while trying not to get any sand on my skin. Having the precut wafers and closed ended pouches made all the difference in the world.
 The last day on the river was a half day. Once we got off the boats we are onto a bus for three hours. Luckily there was a real bathroom stop. Here I just switched out bags. We got back to the hotel and into the shower I went. I had so much adhesive on my skin. I used a ton of adhesive remover, then took a face cloth and washed the whole area. My skin looked pretty good for being engulfed in adhesive for 8 days lol. It took a while to get all the adhesive off. It felt amazing when it was. Obviously, when I got out of the shower I dried off and put on a new ring, wafer and bag, no brava strips. My skin was very happy for this.
The last day on the river was a half day. Once we got off the boats we are onto a bus for three hours. Luckily there was a real bathroom stop. Here I just switched out bags. We got back to the hotel and into the shower I went. I had so much adhesive on my skin. I used a ton of adhesive remover, then took a face cloth and washed the whole area. My skin looked pretty good for being engulfed in adhesive for 8 days lol. It took a while to get all the adhesive off. It felt amazing when it was. Obviously, when I got out of the shower I dried off and put on a new ring, wafer and bag, no brava strips. My skin was very happy for this.
I am so thankful that I did not let having an ostomy get in the way of me missing out on this awesome adventure. I refuse to let anything get in my way of living. I attribute the success of this trip to closed-ended bags, precut wafers, being organized but also for patting myself on the back and having an awesome attitude.
It’s summer and you should not let your ostomy stop you from swimming, exercising and having fun in the sun. Sweat and lots of time in the water can decrease the number of days between pouching system changes for some but there are some simple things you can do that can help. Elaine shares in this video several tips to get your wafer to stick longer. Check out her advice to prolong adherence of your ostomy pouching system especially when swimming, exercising and sweating more this summer.
UOAA also has more information on swimming and advocacy tools for any issues with access in public facilities.
Make sure to grab your FREE GUIDE: ‘3 simple ways to eliminate fears about your ostomy” by visiting Elaine’s website www.ElaineOrourke.com
Elaine O’Rourke is the creator of the program “Surviving To Thriving: Overcoming Ostomy Challenges So You Can Live a FulFilling Life”. She is a certified Yoga Therapist & Teacher since 2003, Sound Healer, EFT & Reiki Practitioner, Recording Artist and International Retreat Leader. Her lighthearted and fun personality shines through her teachings/programs as she loves to inspire others. She is a contributing writer to the national Phoenix Magazine and UOAA, presenter at the UOAA National Conference and speaker at Girls with Guts retreat.
Facebook: https://www.facebook.com/ostomyibdlife/
Instagram: https://www.instagram.com/elaineorourkeyoga/
Email: Elaine@ElaineOrourke.com
Living with an Ostomy and IBD led her to become an Unexpected Beauty Queen and Advocate
Hi Everyone! My name is Robin Brown, I’m a 40-year-old wife, momma & farm girl. I also happen to have an ostomy and the title of Mrs. Washington World America!
My relationship with my guts has been a long battle….even as a child I suffered from severe ulcerative colitis symptoms but I wasn’t officially diagnosed until I had my first bowel resection at age 21 as result from an infection following an appendectomy. I lost my marriage and some guts but I finally got some answers…or so I thought. The next ten years were a rollercoaster of medications, treatments, alternative therapy and surgeries(15 to be exact.)
 I was miserable. My family was miserable. But, I’d had enough and didn’t want any more treatments. Soon I was back in the hospital and one doctor reviewed ALL my info and said he knew exactly how to fix me…OK, just one more surgery then. Well, he was right…he fixed me!! I was no longer having incontinence issues, I could eat again (personalized diet plan) and was feeling great compared to the previous ten years. End of story right?!
I was miserable. My family was miserable. But, I’d had enough and didn’t want any more treatments. Soon I was back in the hospital and one doctor reviewed ALL my info and said he knew exactly how to fix me…OK, just one more surgery then. Well, he was right…he fixed me!! I was no longer having incontinence issues, I could eat again (personalized diet plan) and was feeling great compared to the previous ten years. End of story right?!
WRONG! Less than a year after surgery I was in an accident where I was crushed between our off-road truck and the back wall of our garage. It was a literal and figurative blow that nearly took my life. I had holes in my large intestine, holes in my small intestine, a shattered pelvis, four broken bones in my back and an aortic aneurysm. I had to undergo countless operations, hours of physical therapy and I was even put into a coma while doctors worked fixing one piece at a time.
After everything began to heal I realized how broken I was. After the accident, I lost myself. I had worked as a medical assistant for years and loved working in healthcare. Now that was gone. I was finally a mother after trying for nearly ten years. Now I couldn’t even lift my two-year-old son for a hug. I took great pride in being a partner to my husband. Now I needed him to help me sit on the toilet. I was stressed and depressed. My UC symptoms worsened by the day and now that I had shortened guts it caused a multitude of other problems like rectal prolapse (twice!) which led me to finally agree to get my colostomy pouch. I cried, a lot.
Being home, then in and out of the hospital, and no longer able to have a 9-5 job I decided to start a little online business selling skincare and cosmetics. Not really to make money but just to feel like I was doing SOMETHING! I had to get out of this funk. I was hiding. Hiding from my husband, even though he had an easier time accepting things than I did. Hiding from my reflection- because every time I saw myself I felt depressed and sad. I was hiding from the world by wearing bulky sweatshirts in the middle of summer so no one would see my bag. Then one day in my online makeup group I shared a bit of my story. The response was amazing and beautiful and that’s when things began to shift. One afternoon I received a message from an old friend suggesting I compete in a Mrs. Beauty pageant since the focus is so much on what you do to inspire rather than just what you look like. Me? In a pageant? Probably not. Then a few weeks later the same suggestion from another. Ok universe…I hear you. I decided to apply for the Mrs. Washington America pageant and was quickly named Mrs. Mason County.
Great! What in the heck did I sign up for? Before surgery, I swore off swimsuits and anything tightly fitted. Now, not only will I wear a swimsuit on stage but I’m going to ask to be JUDGED?!?! What on earth was I thinking? Now, in addition to volunteering and fundraising, each queen must have a platform. Something they want to bring awareness to and are passionate about. The obvious choice for me was gastrointestinal disease and ostomy awareness and education, but that’s not the most beautiful platform and can make people uncomfortable. As quickly as the idea came, fear and doubt began to creep in and I promptly began thinking of other ideas.
At my first pageant event, a holiday party to meet all the other queens, we were introduced to a designer that would be custom designing an opening number dress for each of us! As I chatted with the designer I quietly mentioned I had a colostomy bag and could we design something to hide it as much as possible because I wanted to feel beautiful. A short while later I bumped into a sister queen at the elevators. She introduced herself and wanted to know if she could ask a personal question…of course, I said! She asked if she overheard my conversation correctly that I had a colostomy bag? Yes, yes I do! “Really?!? Where, I don’t see it?” She continued, “are you happy you made that choice? What’s the hardest part? Does it hurt?” A million questions rolled off her tongue at once and then she shared her struggles with GI disease and the fact that an ostomy has come up in her doctor’s appointments and she was terrified and thought life would be over¬– until she met me! I knew right then, I had the right platform and that by sharing my story I could help others in ways I never dreamed.
At that moment a woman approached. She wanted to let me know her husband has an ostomy and seeing me on stage gave them so much hope and even though I didn’t win they were cheering for me! Again, I had to thank the universe for letting me know I was exactly where I was supposed to be.
In the months leading up to the pageant, I began volunteering at hospitals and schools, sharing about differences and acceptance. I had the opportunity to be a speaker with a major medical company to share my ostomy journey and provide input to how they can better serve our community. I even went live on Facebook and showed my bag to the world!
In a few short months, I became empowered and proud of my body and my spirit again. I walked the stage in a swimsuit like I was a supermodel, rocked a gorgeous FITTED gown with grace, and with a smile heard myself say the word bowels, as it proudly rang through the pageant auditorium.
 Guess what? I didn’t win. I did not even place in the top 10. I went to the coronation party with a stage smile and promptly excused myself with my best friend by my side. She knew I needed to cry. As we reached the bottom of the grand staircase I could feel the tears of disappointment welling, and her hand grasping tighter to my arm letting me know I just had to keep it together for a few more seconds. At that moment a woman approached. She wanted to let me know her husband has an ostomy and seeing me on stage gave them so much hope and even though I didn’t win they were cheering for me! Again, I had to thank the universe for letting me know I was exactly where I was supposed to be.
Guess what? I didn’t win. I did not even place in the top 10. I went to the coronation party with a stage smile and promptly excused myself with my best friend by my side. She knew I needed to cry. As we reached the bottom of the grand staircase I could feel the tears of disappointment welling, and her hand grasping tighter to my arm letting me know I just had to keep it together for a few more seconds. At that moment a woman approached. She wanted to let me know her husband has an ostomy and seeing me on stage gave them so much hope and even though I didn’t win they were cheering for me! Again, I had to thank the universe for letting me know I was exactly where I was supposed to be.
Soon after, I applied to represent Washington at the Ms. World International pageant after a few weeks and committee meetings later, I was selected! I am now Mrs. Washington World America and I couldn’t be more proud to represent my state and the ostomy community at the upcoming pageant.
I never thought I’d have an ostomy. I never dreamed this farm girl would be a beauty queen. I never imagined my trials would become my triumph and my story of hope. Throughout my life, many have attempted comfort me with the words “everything happens for a reason.” This honestly just kept me waiting for a moment of clarity and answers but that moment never came. I found no reason! I think sometimes bad things just happen and it’s up to us to give them meaning and purpose. For me this is it. Sharing my story, my triumphs, my tragedies. All in the hope that it can be a light for someone stumbling in the darkness.
Robin Brown will be this year’s Ostomy Awareness Day Champion for UOAA. Check out all the ways to get involved and join with her on Saturday, October 3, 2020.
A patient who did not know what to expect walks you through the process (with photos)
By AnneMarie Finn
According to UOAA information on this website, a urostomy is “a surgically created opening in the abdominal wall through which urine passes. A urostomy may be performed when the bladder is either not functioning or has to be removed. There are several different types of surgeries, but the most common are ileal conduit and colonic conduit. Reasons for surgery include bladder cancer, spinal cord injuries, malfunction such as chronic infection of the bladder and birth defects such as spina bifida.” Great definition, but what does it mean? When I was told I would need a radical cystectomy, leading to an ileal conduit I had no clue. The following is my experience.
Because of bladder cancer, my bladder needed to be removed and a new way to pass urine created. Due to the location of the tumor, my urethra was also removed so my surgeon and I settled on an ileal conduit, a conventional urostomy. It is called ileal conduit because a piece of the ileum, or small bowel, is used to make a passage for urine to go from the kidneys and ureters out of the body. The other end is brought out through a hole in the abdomen where urine exits through a stoma (more on that shortly). It is known as an incontinent urinary diversion because you cannot control the urine. As a result, a collection bag or pouch hangs from your abdomen to catch the urine. The pouch is not visible as it is worn under your clothes. Still not clear? It wasn’t for me either.

A couple of days before surgery, I met with an ostomy nurse at the hospital where I would be receiving my surgery. She marked where the stoma would be placed. She saw how I wore my pants. She had me sit, stand, lay down, and bend over, She drew a mark with a marker about 2.5 inches to the right and 3 inches down from my navel and covered it with a waterproof dressing. This would guide the surgeon as to the optimal spot to place the stoma. The surgeon had the ultimate call on where the stoma went, depending on the surgery itself. I also met with a nurse for a pre-op appointment. They went through the typical exam and then explained the ERAS protocol to me. ERAS, Enhanced Recovery After Surgery, is used at my hospital for radical cystectomies. They no longer use a bowel prep. You drink a high carbohydrate drink in the hours prior to your surgery. They get you up walking and feed you by the day after surgery. The goal is to keep your bowels working. This reduces the length of hospital stay and the number of complications.
This is major surgery. It is considered one of the most complex cancer surgeries performed. My surgery took 7 hours. They removed the bladder, urethra, uterus, cervix, fallopian tubes, an ovary, and some lymph nodes. When I woke up, I had a bag, a large incision with more than 30 staples and a Jackson Pratt (JP) drain on my abdomen. I also had intermittent pneumatic compression (IPC) devices on my legs, my spa legs. Blood clots are a common side effect of a radical cystectomy. Because of that, I also received daily prophylaxis blood thinner shots in my belly for 30 days.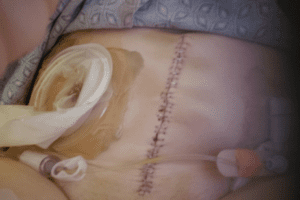 I was not in a great deal of pain which was easily managed with Tylenol. I was definitely weak, but otherwise ok. I went home in 4 days, on my own with my urostomy.
I was not in a great deal of pain which was easily managed with Tylenol. I was definitely weak, but otherwise ok. I went home in 4 days, on my own with my urostomy.
The stoma is the badge of the urostomy. My stoma is about one inch in diameter. It is pretty round, It sticks out. It sometimes moves in and out. You can’t feel it. It has been described as looking like a rosebud. It is red. This is where the urine exits the body. You have no control over it. Sometimes it will also expel mucus. Some people name them. I did.
 Rudolph, my red, round stoma
Rudolph, my red, round stoma
You use a urine collection pouch, or bag, to catch the urine. The hospital will send you home with some so you do not need to have them on hand before you get home. There are many different brands. In fact, until I found what worked best for me, I tried most of them. My pouch is about 8 inches long, 6-7 inches wide and has a 1-2 inch closable spout on the bottom. It also is a deep convex bag as my stoma does not stick out very far and it helps protect my skin. I prefer the clear bag so I can see the stoma and center it when I put it on. There are both one and two-piece bags. I have used both. One-piece pouches have the bag and a skin barrier attached. The skin barrier has adhesive, also called a flange or wafer, that sticks to your skin. There is a hole that goes over the stoma. Some are pre-cut, some are not. If not, you must cut a hole slightly bigger than your stoma before putting it on. There are also two-piece systems. The bags are separate from the skin barrier. They are attached by a Tupperware-like seal. You can leave the skin barrier on and take off the pouch.

Front and back of 1 piece, deep convex pouch
I change my pouch every 3 days. I like to remove the old pouch and take a shower with it off. I feel so free. To remove, I use an adhesive removal spray and wipes to clean the skin. I shower and wash the area around the stoma with soap and dandruff shampoo, which contains Zinc. Some people wash with a vinegar and water combo. If I change without showering, I just use plain water to rinse. After showering, I use a hairdryer on the lowest setting to dry the skin around the stoma so the wafer sticks to it. Drying your skin is important. I have some skin issues so I also use a skin barrier protective sheet, that I cut a hole to match the opening of the wafer, and a cohesive seal.

Protective Sheet with hole cut out and Cohesive Seal
Some people use powders, paste, barrier wipes, etc. I do not. It took a lot of trial and error to find what worked best for me. You need to find what works for you. One of the best ways to do this is to work with an ostomy nurse. They can help you navigate ordering and finding the best system for you.
At night, I use the urinary drainage bag they sent me home with from the hospital. For me, it works the best. There are several brands of night bags and even jugs. I put it on the floor next to my bed inside of a small wastebasket. This has been key as the drain has opened (or been left open) and the wastebasket collected the urine, preventing a rug catastrophe. I am a very active sleeper and I am not really hindered too much from my bag. I am able to sleep on my back, sides, and stomach. Don’t be afraid to sleep. People add their own tubing and tube placement strategies. Use whatever works for you. I also highly recommend a waterproof mattress pad. Mattresses are expensive. I also use the night drainage bag on long car trips. I don’t have to stop and use those disgusting public toilets. I even used it during the Avengers finale. I was probably the only person in the theater who did not have to get up to use the facilities during the movie! People were actually jealous.
 Night Drainage Pouch
Night Drainage Pouch
I honestly can’t even feel my pouch. I empty it every 1-2 hours, depending on how much I drink. Sometimes there is a “ghost” feeling where my bladder used to be making it feel like I have to pee. Ah, the good old days. It is actually a weird sensation drinking a lot and not feeling like I have to go. The bag is not noticeable under my clothes. I really do wear what I wore before surgery: jeans, sheath dresses, shorts, and bathing suits. I am still sexually active. Having gone through this experience with my wonderful caregiver, my husband, has brought us closer. Most importantly, I am cancer-free.
Bladder cancer and urostomy surgery do not stop Annemarie from living her best life.
I am a bag lady. I am highly educated and employed, yet carry a bag wherever I go. I don’t leave home without it. Because of bladder cancer, I have a urostomy. Like many other women, it took some time for my diagnosis. At 57, many of the symptoms I experienced were attributed to my age: menopause, UTIs, kidney stones, fibroids, etc. Thanks to the fibroids, I was scheduled for an ultrasound. It was my gynecologist who found the bladder tumor. She referred me to a urologist. In fact, she insisted. Her office called to make sure I followed through. I met that week with a local urologist. He did a scope. I saw him look at the nurse, concern written on both their faces. He started talking about surgery and apologizing for the diagnosis. In my naivete’, I had gone to the appointment by myself. I don’t remember him even saying the words, but I had bladder cancer.
Scans and a transurethral resection of a bladder tumor (TURBT) were scheduled for the following week. Usually an outpatient procedure, I was in the hospital for 4 days due to heavy bleeding after the TURBT. The tumor was large and the doctor couldn’t get it all but he thought it had penetrated the muscle. Unfortunately, the pathology was inconclusive so he did another TURBT the following week. The outcomes were exactly the same so we both decided my best chances were for a second opinion at Dana-Farber Cancer Institute in Boston. Throughout our discussions, he explained what my future might entail. It looked likely that they were going to have to remove the bladder and I would either have a new “bladder” or a bag. Quite honestly, I had no idea what it entailed, but I was horrified.
Dana-Farber is an amazing place. I had a whole team in place: a medical oncologist, an oncology urologist, a nephrologist, among others. The plan was an MRI to confirm the tumor’s pathology, a nephrostomy tube, chemotherapy and, if the cancer had not spread, a radical cystectomy. If it had spread, I would not need surgery but would be eligible for palliative care. Who would have thought surgery is the best case scenario. Due to claustrophobia, and despite anesthesia and Ativan, I moved so the MRI was inconclusive. I needed another TURBT. Thanks to my new amazing surgeon, the tumor was removed and the passage to my kidney was cleared. The pathology of the tumor showed no spread to the muscle and an ultrasound showed no more kidney hydronephrosis. Even better, I would no longer require chemotherapy. I did try immunotherapy with BCG but it did not work. The cancer was aggressive so we had to treat it aggressively. My radical cystectomy was scheduled for January 25, 2019.
It took me a long time to get there. I even asked what would happen if I did not receive the surgery. I would be dead in a year.
Wow, that was sobering. Because of the proximity of the tumor, I did not qualify for a neobladder. I would have to have a urostomy. Every time I talked about it, or even thought about it, I cried. I felt like I was going to be a freak. I offered my husband a divorce if he wanted one. I was devastated and frightened. I have learned that fear of the unknown and our imaginations are far worse than the reality. While so much of what had happened to me was out of my control, I did have control over one thing: HOW I handled everything. I decided knowledge was power. I was fortunate. My hospital had a class for urostomy candidates. For the first time, I was able to see an actual urostomy pouch. I was given hands-on instruction on how to change a bag. I met ostomy nurses (the best people in the world!) who would be helping me.
I decided I would be the one to handle my changes, right from the start. I would take control.
My surgery lasted 7 hours. I needed a transfusion but things went well otherwise. The surgery was not easy. People have described it as feeling like you were hit by a bus. I never really had any pain. It was easily managed with Tylenol. However, I was so weak. I eventually needed an iron transfusion. The one thing I wish I had gotten for my return home was a shower chair. Showers were the worst for me. It took me two months to feel more like myself and another month before I felt ready to return to work. I also cannot say enough about getting a good ostomy nurse. I have been described as a delicate flower (surprising to those who know me). I have very sensitive skin. The nurse was a Godsend to me in trying to manage all of my skin issues. After my visiting nurse visits ended, I continued to see the ostomy nurses at the hospital where I had my surgery. It took a year but, through trial and error, I finally have gotten a handle on things.
I had a few leaks. They were usually caused by user error. They were not the huge floods I expected. Honestly, none of this was as awful as I expected. So many people said this would be my “new normal”. I can’t stand that term. I call it my new reality. There isn’t anything normal about having a urostomy. However, it is very doable. I now wear two-piece bathing suits. I didn’t before. I am wearing the same clothes as I did before. I can kayak, hike, ride my bike, swim for hours, anything I did before. I was here for the birth of my first grandchild. I am back to work, a job that I love. I am not shy about talking about my bag to others. It is not a secret. In fact, I am kind of proud of it. I am alive and life is good.
Imagine being your 15-year-old self again. What did that feel like? Young, carefree, happy…healthy?
For me, I felt all of those things every day. I played the clarinet, got good grades, was athletic from running track, active in school/church clubs and had amazing family/friends. What more could I want as a teenager?
I didn’t want for anything until one day I no longer felt like my healthy self anymore and all I wanted was to be healthy again. This is when my life changed forever…
It was November of 2012, at the time I had just moved to Los Angeles, California with my mother from Maryland. I was very excited to move and support my mom with her new job opportunity. She is like my best friend and nurturer at the same time. It was always just her and I growing up, no siblings. California’s scenery was colorful and vibrant. All I could picture were the great things my future would bring living there.
That picture flipped upside down within weeks. I could feel my stomach expressing to me that it didn’t like the chicken nuggets or the pepperoni pizza, I was feeding it. Sharp pains that felt like knives were sticking me each time I would eat, pushed me to never want to pick up another piece of food again. No over-the-counter medicine could relieve the amount of pain I would feel. Sick little me sat helplessly with my mother by my side in Ronald Regan UCLA Medical Center’s emergency room waiting to be admitted and seen by a doctor. I thought to myself, “What was happening to me? I don’t understand.”
I couldn’t understand. I was just fine a month ago. My mom was just as confused as I was. The doctors weren’t transparent enough with my diagnosis and had trouble figuring out what was the actual problem. After a few tests, I was diagnosed with ulcerative colitis/Crohn’s disease. This diagnosis soon changed once the gastrointestinal team at UCLA Medical Center (UCLAMC) realized it was strictly my colon that was being affected which changed my diagnosis to ulcerative colitis.
I had no idea what ulcerative colitis was nor had I ever heard of it before. My current gastroenterologist, Dr. Ziring, asked who in my family had the disease but I wasn’t familiar with anyone. My father, mother, and grandparents didn’t have any trace of ulcerative colitis. It was concluded that the change in climate and stress could have taken a toll on my body to make me flare-up. I couldn’t eat certain foods anymore. I was prescribed all types of medication that I had never seen and forced to take pills that were pretty huge to swallow.

Lacee Harper with her mother.
Nearly one month spent in the hospital, my routine had changed. I would wake up take my meds first, eat (liquid-solid foods), watch TV, read a book, walk around to gain my strength and repeat at least three times a day. Once I was released, I remember being so happy to be a normal person again. That feeling went away when my mom took me to buy nutritional drinks to restore my protein, vitamins, and minerals. I couldn’t fit into any of my clothes from the amount of weight I lost and my toned body went away. Dr. Ziring told me that I would live with this forever because there is no cure, which I didn’t want to believe. All I could do was try to understand and educate why my body reacted the way it did to certain foods, activities and mental stability.
Fast forward to 2013 where I moved back to Maryland with my mother, I was enrolled back in my previous high school and actively seeing, pediatric gastroenterologist, Dr. Oliva-Hemker at John Hopkin’s hospital. I couldn’t do any of the previous extracurricular activities I participated in and could only workout at a minimal intensity due to my low blood counts. Throughout the school year, I experienced many flare-ups and trial/error with different medications. Some hospitalizations were longer than others and overtime I became stricter with my diet to prevent excessive flare-ups. My high school graduation wasn’t the best time for me because I was experiencing a severe flare-up that interfered with my ability to keep food down. I missed my senior week summer trip to recover in the hospital and get back to feeling better again.
After graduating from high school, I switched gastroenterologists since I was considered an adult. Dr. Rosen had been my mom’s gastroenterologist for years so the transition was smooth. I was stabilized on Humira and Prednisone throughout my community college career. By then, my mother and I had moved to Atlanta where the weather was nicer. I think the weather, being around family/friends and less stress I experienced helped my flare-ups calm down living in Atlanta. I truly enjoyed my time there and experiencing college at Georgia State University, as well as working part-time.

Lacee recently graduated with a master’s degree from the S.I. Newhouse School of Communications at Syracuse University.
Once I completed my first two years of college and received my associate’s degree, I transferred to Syracuse University (SU) to achieve my bachelor’s degree. This was one of the hardest transitions of my life moving from the South to the cold North. My third year of college and first-year being away at a university led to my body experiencing an extreme transition which resulted in three severe flare-ups. My mother left Atlanta and moved back to Maryland to be closer to me because she was terrified of how sick I was getting. Each time I flared up, I flew home to get the treatment from Dr. Rosen. Suddenly, Humira no longer worked for my body anymore and Prednisone wasn’t healthy for me to keep using to reduce inflammation due to its side effects.
During senior year, my 3-week hospitalization interfered with my academics and involvement in extracurricular activities. At this time, I was advised to try Entyvio and I was tired of trying new medications. The only way I could have some quality of life was to remove my colon. My mom was concerned for me, but I couldn’t let her concerns steer my thinking I knew I had to do this for me if I wanted to make it to graduation.
In November of 2017, I set an appointment with Dr. Colvin in Northern Virginia to discuss my surgery. I had the surgery during my college winter break, spent Christmas in the hospital, recovered and returned back to school. At the time, I didn’t know how I was going to apply to graduate school at the S.I. Newhouse School of Communications at SU but I did that during my recovery period. It took a lot of exercise, mental motivation, empathy and support from family, my best friends, mentors and peers at school. With amazing grace and good spirits, I got accepted into the public relations program at the S.I. Newhouse School of Communications.
From this specific point on, learning how to function in everyday life with my ostomy took a lot of patience, time, emotional breakdowns, motivation and positive mental strength. I don’t regret any of it at all. I do not have to worry about missing out or not fully enjoying any more important events of my life. Now as of 2020, I have been medication-free for two full years, graduated school with all of my degrees, feel healthier than ever, working full-time in public relations and am actively pursuing my dreams in the entertainment (modeling/tv/film) industry.
It wasn’t until a couple of months ago, I discovered United Ostomy Association of America (UOAA) and chose to reach out to Advocacy Manager Jeanine Gleba about getting more involved. Since reaching out, I have gained the opportunity to advocate for patient’s access to treatment during the Digestive Disease National Coalition Day on the Hill and spoke on the behalf of UOAA. I am elated to have met UOAA’s team and to represent others like myself who have experienced challenging obstacles.
I couldn’t be more grateful for my ostomy and must say that it changed my life for the good. Life is full of obstacles but how you choose to overcome them will make your life. I chose to take full control of my life in order to have a better quality of life. It doesn’t matter who you are, you can truly do whatever you put your mind to. Believing in yourself and staying grounded in positivity, motivation and dedication is key. Follow your dreams, find what makes you happy and don’t let the negatives take control of your life.
Contact Us
United Ostomy Associations of America
P.O. Box 2293
Biddeford, ME 04005-2293
Call us toll-free at: 1-800-826-0826.
Our Information Line hours are Monday-Friday, 9am to 3pm EST. If you have an emergency, please dial 911 or contact your local medical professional.
Please understand that UOAA is a private, nonprofit, advocacy and informational organization. We are not a medical facility and we do not have medical or legal professionals on staff. Therefore, UOAA does not provide Medical, Mental Health, Insurance or Legal Advice. Visit UOAA Virtual Ostomy Clinic provided by The Wound Company for non-emergency, virtual ostomy support.
Get Involved
UOAA is the leading organization proactively advocating on behalf of the ostomy community. Recognizing that we are always stronger together, we encourage everyone to get involved by joining our Advocacy Network. We’ve also created several Advocacy Tools and Resources to help you successfully advocate on behalf of the ostomy community to ensure every ostomate receives quality care.

