Ostomates often struggle with fashion and feel their options are limited. Without a doubt, part of the journey to adjusting to your ostomy is finding ways to dress yourself that is both comfortable and still allows you to express your individuality. This was no different for Deirdre, who felt that her passion for fashion and style were taken away from her after her ostomy procedure.
Fortunately, clothing designers have recognized that women come in all shapes and sizes, so you can now find pants with a variety of waistline heights. This allows you to find a style to fit your body and your needs. For active wear, consider wearing yoga pants or stretch pants to help support the pouch during exercise. You might also try biker-style shorts since they can be worn alone or layered under shorts, exercise pants or other stretch pants.
Part of adjusting to an ostomy also includes finding the right pouching system that fits you as well. With the help of her stoma care nurse, Deirdre found a pouching system that worked for her, and she regained the confidence to go out, go to work, socialize with her friends, and do all the other activities she dreamed of being able to do when she was in the hospital. For Deirdre, fashion and style are important aspects of her life, so having a pouch that works with different outfits allowed her to feel like herself again. Her journey with chronic illness and living with a stoma has become so much more about self-esteem, body image, and loving herself. According to Deirdre, “Once I went out and started getting back to normal life again, no one ever would’ve known that I had a stoma, because the bag was so easy to wear and was hidden under my clothes.”
Deirdre found a discreet pouching system that fit her well and gave her a feeling of security, which helped her regain the confidence to leave the house in skinny jeans, or even sports leggings. Finding a pouching system with the right fit to Deirdre’s body meant having the confidence to socialize again. Although there may be some styles of clothing you want to avoid after surgery, you still have many choices open to you. See which styles you like the best, and which you find most comfortable. Every body is different and finding the right fit can make the difference between confidence and insecurity.
*Deirdre is a Coloplast product user who has received compensation from Coloplast to provide this information. Each person’s situation is unique, so your experience may not be the same. Talk to your healthcare provider about whether this product is right for you.
Call your healthcare provider if you have any medical concerns about managing your ostomy. You may also contact your Coloplast® Care Advisor for product usage and availability questions at 1-877-858-2656.
Prior to use, refer to the product ‘Instructions for Use’ for intended use and relevant safety information.
Editor’s note: This article is from one of our digital sponsors, Coloplast. Sponsor support along with donations from readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.


 I’m thankful for all of the WOCNs I have been to. Some I’ve known for many years. They are very knowledgeable and helpful with various products.I also want to give a shoutout to our great WOCNs at 11 Health & Technologies for being amazing for our team and patients. ? –Megan Alloway
I’m thankful for all of the WOCNs I have been to. Some I’ve known for many years. They are very knowledgeable and helpful with various products.I also want to give a shoutout to our great WOCNs at 11 Health & Technologies for being amazing for our team and patients. ? –Megan Alloway I want to tell my story concerning my ileostomy in order for people to understand how it is living with one and how a person can live a normal life and more.
I want to tell my story concerning my ileostomy in order for people to understand how it is living with one and how a person can live a normal life and more.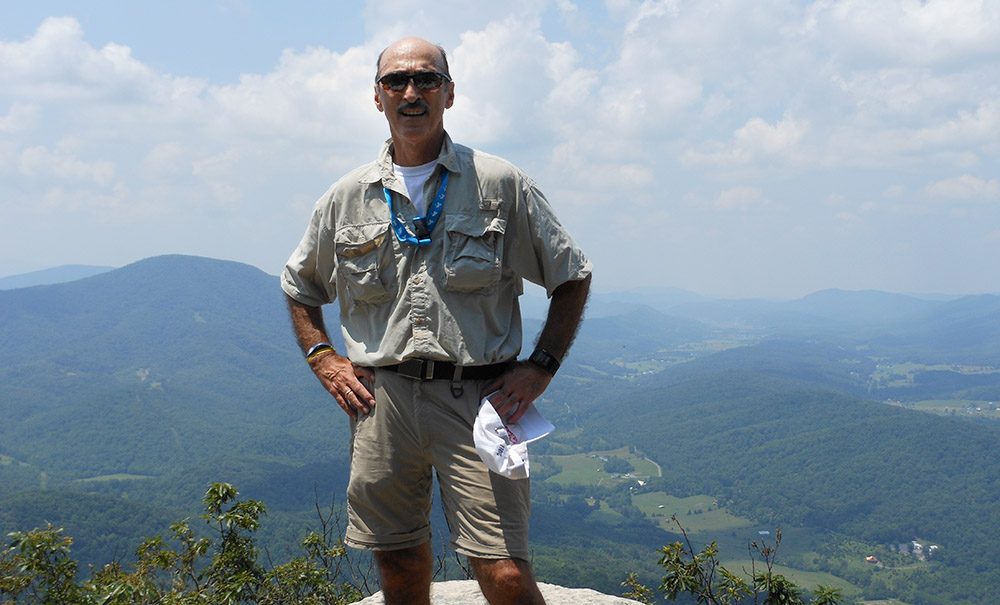


 Along the way, I started to feel strong. I was amazed by what both my body and my mind could accept and turn into a positive. I started to really take care of my physical health, and in the three years that I have been the sickest in my life, I became the most physically strong I have ever been by participating religiously in
Along the way, I started to feel strong. I was amazed by what both my body and my mind could accept and turn into a positive. I started to really take care of my physical health, and in the three years that I have been the sickest in my life, I became the most physically strong I have ever been by participating religiously in 



