Written by Danielle Gulden and Joe Teeters
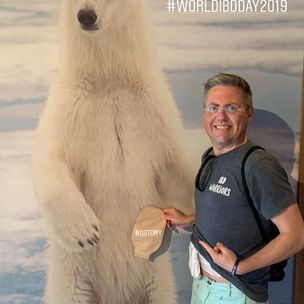
We all know that “laughter is the best medicine”! This year’s Ostomy Awareness Day Champions, Danielle Gulden and Joe Teeters, not only love that phrase, they live it! These two best friends, and co-founders of Double Baggin’ It are IBD warriors and permanent ileostomates. They’re also comedians, speakers and Two Best Friends without Buttholes! They truly believe in the power of laughter, humor, advocacy and awareness! Which is why they LOVE Ostomy Awareness Day! For them, every day is a chance to raise awareness. But Ostomy Awareness Day is a special day to reflect and celebrate their life-saving surgeries and the lives they were given back! They share their stories so that future, new and veteran ostomates know that they are not alone!
Danielle and Joe have each been living with Inflammatory Bowel Disease for over 29 years. Although their IBD and ostomy journeys have been quite different, their positive outlook on life and ridiculous sense of humor are the same!
View this post on Instagram
Prior to 2014, Joe and Danielle had no idea the other existed…so, let’s rewind a few decades and learn about the journey of each of these Two Best Friends Without Buttholes!
Growing up, Danielle was a very healthy child, an extremely outgoing teen, and an adventurous free spirit! Spontaneity was her specialty, and travel was always her first love! Joe, on the other hand, always had “poop problems.” He was always pooping and known as “Joe the Pooper” by his siblings. Like Danielle, he was an outgoing, active, and social teenager.
Fast forward to Danielle’s late teens and early 20s. By the time she was a sophomore at The Ohio State University, Danielle’s health drastically changed! She saw her busy social life dissolve; she’d make plans and have to cancel. Spontaneity was no longer an option, and the idea of traveling was now a nightmare!
Danielle had to drop out of classes because of her poor health. Her symptoms and pain were becoming harder to ignore. She was in the bathroom around 25 times a day and became extremely malnourished and anemic.
You can hide your bag, but don’t ever let your bag hide you!
After being misdiagnosed for 6 years with a gluten intolerance, a colonoscopy in April of 1999 showed severe ulcerative colitis. From 1999 until 2007, Danielle’s life was a constant barrage of colonoscopies, radiological tests, bloodwork and pharmaceutical cocktails. She did the research and finally decided to have ostomy surgery.
After high school, Joe enlisted in the Naval Reserves. He passed the military physical and was cleared for training. While away, Joe’s poop problems became more pronounced, and the pain was gradually becoming more than just an annoyance.
When he returned home after 5 months, he was in the best physical shape of his life. On the outside he looked healthy, but inside something was wrong. Joe was initially diagnosed with irritable bowel syndrome, then a colonoscopy in 1993 lead to his diagnosis of severe Crohn’s Disease. Two years later he had his first intestinal resection. Joe’s Crohn’s continued to advance, and he had a second intestinal resection in October of 2004. 
Back in Cleveland, Danielle was super excited for her ostomy surgery! She was ready to stop being a prisoner to her bathroom and get back to living her life to the fullest! On April 30th, 2007, Danielle had her total proctocolectomy with end ileostomy at the Cleveland Clinic. It was truly one of the greatest days of her life! She high fived every single person on the way to the OR.
From day one, she embraced her ostomy, and her new life as an ostomate. Within a month or two of her surgery, Danielle was back to exploring and enjoying her pre-sickness hobbies and joys. She traveled, hiked, camped, swam, went to concerts, and amusement parks. Life was good again! She also joined the Cleveland chapter of the UOAA and eventually became active on their executive board.
Fast forward a few years, and 120 miles away in Columbus, Ohio. Within a year of his second resection, Joe’s rectal Crohn’s disease became severe, and his rectum very strictured. After consulting with his GI and surgeon, Joe had a full proctocolectomy with end ileostomy on December 27th, 2012.
Joe’s recovery process and post-surgical experience was very different from Danielle’s. In addition to becoming an ostomate, the amount of bowel he had lost from three surgeries left him with Short Bowel Syndrome. It took the better part of a year to fully recover and return to pre-surgery activities.
During Joe’s recovery, a Facebook support group for ostomates became a lifeline. It was a great source of inspiration and hope, and a wonderful place that showed him he was not alone. Later, he sought out Central Ohio United Ostomy Association support group and became a member of the organization.
By now, you must be wondering how the heck these Two Best Friends Without Buttholes finally met. As you can see, they have traveled separate but similar paths in their battles with Crohn’s and ulcerative colitis. Their paths crossed in that Facebook support group mentioned earlier, when Danielle posted that she and her family were relocating to Columbus, Ohio. Joe, being a Columbus resident, and fellow ostomate, reached out and introduced himself. After meeting in person, in late 2014, at their local UOAA Affiliated Support Group, they started hanging out after the meetings. They soon discovered that they had a very similar outlook on life and shared a ridiculous sense of humor, and they wanted to use that to help others. A best friendship began…and slowly but surely, their vision for Double Baggin’ It was coming together. They decided to go to the United Ostomy Associations of America’s National Conference in September of 2015. There, after meeting over 400 ostomy patients like themselves, they decided to stop dreaming and start making their vision for Double Baggin’ It a reality. Double Baggin’ It was born, that week, when they filmed their first DBI video on a rooftop in downtown St Louis, Missouri.
Through Double Baggin’ It, Danielle and Joe use their humor, wisdom, and stories to connect with and support other people living with ostomies and Inflammatory Bowel Disease. They advocate and raise awareness at the local and national level for both United Ostomy Associations of America and the Crohn’s and Colitis Foundation. Danielle and Joe also visit with their legislators yearly in Washington, DC to share their voices and stories.
You can find them on Facebook, Instagram, TikTok, Twitter and YouTube (@DoubleBagginIt) where you can watch them raise awareness through shenanigans and ostomy-bombing (placing an ostomy bag on a statue, landmark, anywhere they see fit!) They also can be found speaking at IBD and ostomy conferences, support groups, camps, hospitals and classrooms – sharing their stories and spreading laughter through improv. Danielle and Joe know that not everyone is comfortable rocking out with their bags out – and that’s totally ok! What these Two Best Friends Without Buttholes want to make perfectly clear, is that “You can hide your bag, but don’t ever let your bag hide you!”
Join with this year’s Ostomy Awareness Day Champions in spreading awareness by following Double Baggin’ It and UOAA on social media and visiting the Ostomy Awareness Day page to keep up to date on all the latest events.

 saved her life. She also wants to serve as an inspiration to other young people facing similar challenges and let them know they can “live the life they want because of the ostomy bag” and not in spite of it. Sydney exemplifies the resilience of the ostomy community.
saved her life. She also wants to serve as an inspiration to other young people facing similar challenges and let them know they can “live the life they want because of the ostomy bag” and not in spite of it. Sydney exemplifies the resilience of the ostomy community.
 from wonderful WOC nurses, experienced ostomates, amazing doctors and dedicated advocates.
from wonderful WOC nurses, experienced ostomates, amazing doctors and dedicated advocates. The event will come to a close with a special presentation from Magen Cherry, a j-poucher and winner of the 2007 Miss Texas USA competition. She uses her platform to share encouragement and bring hope to fellow ostomates and j-pouchers coming to terms with their new reality. Fun fact: Magen had a colonoscopy three days after being crowned Miss Texas USA!
The event will come to a close with a special presentation from Magen Cherry, a j-poucher and winner of the 2007 Miss Texas USA competition. She uses her platform to share encouragement and bring hope to fellow ostomates and j-pouchers coming to terms with their new reality. Fun fact: Magen had a colonoscopy three days after being crowned Miss Texas USA!
 First off, I accepted the fact early on that I was going to have an ileostomy for the rest of my life because it was a decision I made for a better quality of life. After accepting it, I could focus on moving forward versus dwelling on the “how’s” and “why’s” with ulcerative colitis.
First off, I accepted the fact early on that I was going to have an ileostomy for the rest of my life because it was a decision I made for a better quality of life. After accepting it, I could focus on moving forward versus dwelling on the “how’s” and “why’s” with ulcerative colitis.


 pantyliners in my underwear. When I retired from active duty in August 1996, I immediately started my second career as an Army JROTC Instructor in Bennettsville SC. I continued to go to the bathroom quite frequently and in the spring of the following year my daughter, who was six at the time, wanted me to play horsey with her and take her around the block. I bent down half in tears and told her that “daddy can’t play horsey because he is too sore on his bottom”. I immediately went to talk to my wife and we both agreed it was time to get back to having an ostomy bag. That summer at the Columbia SC Veterans Administration hospital, I had my third surgery to restore my ostomy due to my poor quality of life with the J Pouch. On the positive side, since I’ve had an external pouch, the veteran’s administration awarded me 100% total and permanent disability. I spent the next 23 years as an Army JROTC Instructor.
pantyliners in my underwear. When I retired from active duty in August 1996, I immediately started my second career as an Army JROTC Instructor in Bennettsville SC. I continued to go to the bathroom quite frequently and in the spring of the following year my daughter, who was six at the time, wanted me to play horsey with her and take her around the block. I bent down half in tears and told her that “daddy can’t play horsey because he is too sore on his bottom”. I immediately went to talk to my wife and we both agreed it was time to get back to having an ostomy bag. That summer at the Columbia SC Veterans Administration hospital, I had my third surgery to restore my ostomy due to my poor quality of life with the J Pouch. On the positive side, since I’ve had an external pouch, the veteran’s administration awarded me 100% total and permanent disability. I spent the next 23 years as an Army JROTC Instructor.
 intestine and the weak spot is in the same area the surgeon created your stoma.
intestine and the weak spot is in the same area the surgeon created your stoma.


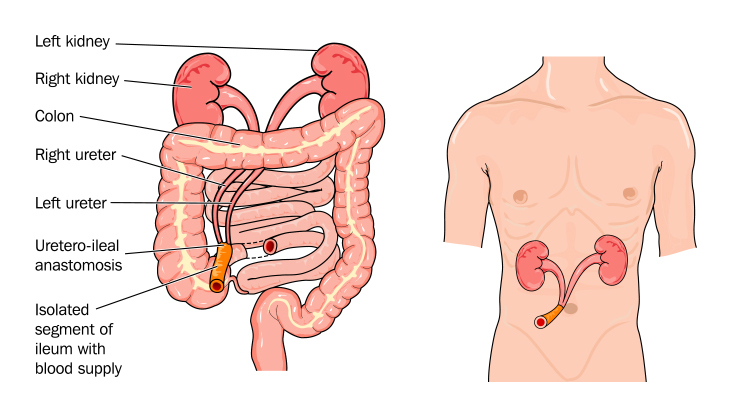 Why Do People Need A Urostomy?
Why Do People Need A Urostomy?


