 My journey with Short Bowel Syndrome (SBS) spans 61 years, and it has been full of twists and turns. I’ve often wished that I understood from the beginning exactly what it meant to have SBS – it is not temporary, rather it is chronic. That means it’s a lifelong condition, and it has frequently caused me to make adjustments to maintain my independence and lead a productive and meaningful life. Reaching independence and self-reliance took years of learning the importance of self-advocacy to get the information I needed from my healthcare providers, no matter how difficult it may have been to hear that information. Each symptom, diagnosis, ostomy and medical procedure that preceded my eventual SBS diagnosis posed new challenges. The more I knew about what lay ahead for me, the more I could take charge of my own life. As August marks SBS Awareness Month, I hope my experiences will help inform and inspire others living with this serious and chronic malabsorption disorder to speak up and ask for information and tips to help maintain as much independence as possible.
My journey with Short Bowel Syndrome (SBS) spans 61 years, and it has been full of twists and turns. I’ve often wished that I understood from the beginning exactly what it meant to have SBS – it is not temporary, rather it is chronic. That means it’s a lifelong condition, and it has frequently caused me to make adjustments to maintain my independence and lead a productive and meaningful life. Reaching independence and self-reliance took years of learning the importance of self-advocacy to get the information I needed from my healthcare providers, no matter how difficult it may have been to hear that information. Each symptom, diagnosis, ostomy and medical procedure that preceded my eventual SBS diagnosis posed new challenges. The more I knew about what lay ahead for me, the more I could take charge of my own life. As August marks SBS Awareness Month, I hope my experiences will help inform and inspire others living with this serious and chronic malabsorption disorder to speak up and ask for information and tips to help maintain as much independence as possible.
A very long time ago, before cellphones, DVD players, home computers, microwaves and color TV, I was born in New Jersey in February 1959. I was a very “clean” baby, with no dirty diapers, which soon raised concern among the medical professionals who started me on enemas and laxatives. I ate very little and projectile vomited most of what I did eat. My mother continuously tried to find out what was wrong with me. Despite many doctors advising her that it was a discipline issue, no diagnosis made sense. None of their theories panned out. Nothing worked. And so began a long journey of wishing we had known what I was living with much earlier on.
In the summer of 1963, my mother, in her desperation, called the White House, spoke to the switchboard operator and requested the name of the Kennedy children’s pediatrician. She then made an appointment with the chief of pediatric surgery. The doctors conducted multiple tests, but unfortunately, I was discharged before the test results were back as the hospital was dealing with another emergency patient! Consequently, my mother did not receive the results, and we left wishing we had more answers.
It took three more years, another hospitalization and my first surgery for a doctor to request those records and discover I should have been diagnosed with a rare, congenital condition called Hirschsprung’s disease back in 1963. Back then, my family and I didn’t know that this diagnosis would increase the likelihood of future gastrointestinal procedures and diagnoses, including SBS. In fact, after that first surgery, my doctors told me I would be fine. Yet, I developed a fistula and the treatment/surgery for that left me with an ostomy. It closed within a year, and my parents were told yet again that I was fine, and we had learned all we needed to know.
Throughout my childhood, I continued to experience episodes of vomiting and few bowel movements, which left me very thin. To stop the vomiting, I had a laparoscopic procedure as a young adult, which I hoped would be the last of my surgeries – if only I had known what lay ahead. My surgeries did not stop there as I had hoped, and I had a second and third ostomy. In 2002, I was placed on total parenteral nutrition (TPN) for the first time. At that time, I was only receiving TPN during my stay in the hospital while recovering from surgery. My body had tried to cover up the symptoms of malabsorption for more than forty years, and I was now seeing the effects of my severe nutritional deficits. I would return to needing TPN periodically over the next two decades.
In graduate school, I met my husband, and we now share a wonderfully supportive family. When we wanted to start a family, there were some severe issues with my pregnancies. My firstborn was delivered via emergency caesarean because I couldn’t stop vomiting. I was hospitalized seven times during my second pregnancy. And then when I finally went into labor, my blood pressure dropped drastically throughout the delivery. I’m happy to say that despite their dramatic entrances, my daughters are happy, healthy and successful – both are biomedical engineers, and one is also a doctor.
In April 2006, I participated in a colonic motility study, and what I’d learned in pieces over the years was finally confirmed: my colon was functionally deficient.  Six years later, I found myself unable to eat due to severe abdominal pains and a pseudo-obstruction and was put back on TPN. I feared this would prevent me from traveling on a three-week family trip to Australia, but my husband and daughters learned how to properly store, prepare and administer my TPN infusions, so we could still travel. I am so grateful to have been able to enjoy that trip with my family despite my TPN, ostomy and needing to use a catheter. I would encourage families and caregivers of people living with ostomies and/or SBS to take every opportunity to promote their self-care and independence as much as possible. For me, traveling with my family is important. Learning how to pack and plan our trips in ways that help me maintain my independence has made a big difference.
Six years later, I found myself unable to eat due to severe abdominal pains and a pseudo-obstruction and was put back on TPN. I feared this would prevent me from traveling on a three-week family trip to Australia, but my husband and daughters learned how to properly store, prepare and administer my TPN infusions, so we could still travel. I am so grateful to have been able to enjoy that trip with my family despite my TPN, ostomy and needing to use a catheter. I would encourage families and caregivers of people living with ostomies and/or SBS to take every opportunity to promote their self-care and independence as much as possible. For me, traveling with my family is important. Learning how to pack and plan our trips in ways that help me maintain my independence has made a big difference.
In August 2013, I was once again faced with just how much I didn’t know about my condition when I was officially diagnosed with SBS. My doctor explained that, rather than solely due to the length of my bowel, my SBS diagnosis was based on my clinical symptoms. My intestines could not sufficiently absorb the nutrients my body needed, leading to malnutrition and dehydration. To maintain nutrition, I continued on TPN.
After finally reaching 145 pounds in September 2019, I was told to discontinue TPN. With SBS, however, I do not know how long this reprieve will last, and these unknowns are important motivators for me to self-advocate when it comes to talking to my healthcare providers. As much as possible, I think healthcare providers should be upfront about the ramifications of living with SBS to fill the gaps in understanding disease management. For me, I spent a lot of time learning as I went along, and my hope is that by sharing my experiences, I can encourage others to ask the tough questions every step of the way.
I am thankful my husband and daughters have always been there for me, helping me emotionally at every doctor’s visit. My husband especially helps me get through each learning curve and the occasional late-night clean-up from messy ostomy accidents. I even have a service dog who carries my medicine for me wherever I go – I consider him my personal ambulance. Without this wonderful support around me, my life would be much more complicated.
That support has helped me take an active role in advocating for myself and others with ostomies, feeding tubes and other GI issues. Each condition differs in how they affect us physically, yet many of us share common concerns. Though people like me may appear healthy on the outside, I want to increase awareness that SBS can be a hidden illness requiring a lot of medical maintenance, sometimes including an ostomy and feeding apparatus. I want to support those like me who also may feel overlooked. Because of that, I started a support group that focuses on ways to continue living our lives, discussing everything from travel to preparing for emergencies. I also advocate on the national level, attending National Institutes of Health conferences in Washington, D.C. I would encourage patients and caregivers to attend local support groups as well as regional and national conferences to meet other people with SBS to share experiences and tips.
These opportunities to connect with the community of patients and caregivers managing GI conditions help to remind me I am not alone. Our individual journeys to SBS diagnosis may involve varied GI conditions and symptoms, and it can feel challenging to find others who share our experience. Sometimes our family and friends forget that we are not quite as physically strong or have stamina unless we mentally prepare ourselves for individual occasions. But in our shared SBS community, we can truly feel related to, supported and understood. I may not have had all the answers along the way, but with support and community I don’t have to dwell on what I wish I had known. I can simply live and learn through each moment.
To join the community and learn more about others living with Short Bowel Syndrome (SBS), visit https://www.facebook.com/TakedaSBS. You can also engage with #shortbowelsyndrome on social channels, especially during the month of August, which is SBS Awareness Month.
This article was created and sponsored by Takeda.
Editor’s Note: This educational article is from one of our digital sponsors, Takeda. Sponsor support along with donations from our readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.




 My journey with Short Bowel Syndrome (SBS) spans 61 years, and it has been full of twists and turns. I’ve often wished that I understood from the beginning exactly what it meant to have SBS – it is not temporary, rather it is chronic. That means it’s a lifelong condition, and it has frequently caused me to make adjustments to maintain my independence and lead a productive and meaningful life. Reaching independence and self-reliance took years of learning the importance of self-advocacy to get the information I needed from my healthcare providers, no matter how difficult it may have been to hear that information. Each symptom, diagnosis, ostomy and medical procedure that preceded my eventual SBS diagnosis posed new challenges. The more I knew about what lay ahead for me, the more I could take charge of my own life. As August marks SBS Awareness Month, I hope my experiences will help inform and inspire others living with this serious and chronic malabsorption disorder to speak up and ask for information and tips to help maintain as much independence as possible.
My journey with Short Bowel Syndrome (SBS) spans 61 years, and it has been full of twists and turns. I’ve often wished that I understood from the beginning exactly what it meant to have SBS – it is not temporary, rather it is chronic. That means it’s a lifelong condition, and it has frequently caused me to make adjustments to maintain my independence and lead a productive and meaningful life. Reaching independence and self-reliance took years of learning the importance of self-advocacy to get the information I needed from my healthcare providers, no matter how difficult it may have been to hear that information. Each symptom, diagnosis, ostomy and medical procedure that preceded my eventual SBS diagnosis posed new challenges. The more I knew about what lay ahead for me, the more I could take charge of my own life. As August marks SBS Awareness Month, I hope my experiences will help inform and inspire others living with this serious and chronic malabsorption disorder to speak up and ask for information and tips to help maintain as much independence as possible. Six years later, I found myself unable to eat due to severe abdominal pains and a pseudo-obstruction and was put back on TPN. I feared this would prevent me from traveling on a three-week family trip to Australia, but my husband and daughters learned how to properly store, prepare and administer my TPN infusions, so we could still travel. I am so grateful to have been able to enjoy that trip with my family despite my TPN, ostomy and needing to use a catheter.
Six years later, I found myself unable to eat due to severe abdominal pains and a pseudo-obstruction and was put back on TPN. I feared this would prevent me from traveling on a three-week family trip to Australia, but my husband and daughters learned how to properly store, prepare and administer my TPN infusions, so we could still travel. I am so grateful to have been able to enjoy that trip with my family despite my TPN, ostomy and needing to use a catheter. 




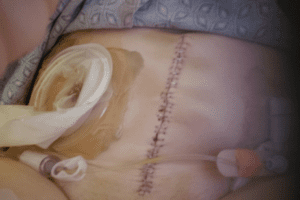 I was not in a great deal of pain which was easily managed with Tylenol. I was definitely weak, but otherwise ok. I went home in 4 days, on my own with my urostomy.
I was not in a great deal of pain which was easily managed with Tylenol. I was definitely weak, but otherwise ok. I went home in 4 days, on my own with my urostomy. Rudolph, my red, round stoma
Rudolph, my red, round stoma

 Night Drainage Pouch
Night Drainage Pouch

