Barbara Dale, RN, CWOCN, CHHN, COS-C
Director of WOC Services at Quality Home Health
Jeanine Gleba UOAA Advocacy Manager
I am a Wound, Ostomy, Continence (WOC) nurse in a rural home health agency. I have worked in the home health field since 2001. Many times when I visit patients in their homes, they complain about the lack of knowledgeable ostomy nurses in the facility (e.g., hospital) they came from or even from my own agency. I try to explain to them that ostomy care is specialized and in general nurses don’t get much (if any) training in nursing school for this type of medical condition. I compare this with my own lack of IV education and skills since I rarely do labs or port flushes and have lost many of my previous skills. We can’t all know everything about all aspects of medical care and not every agency has access to an ostomy trained or ostomy certified medical provider. Nonetheless, it is the home health agency’s responsibility when they accept you as a patient to provide you the care you need and deserve. You have a right to quality care.
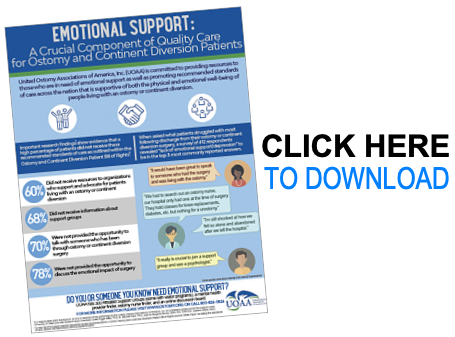
Are you aware of the patient bill of rights (PBOR) for persons with an ostomy or continent diversion? United Ostomy Associations of America (UOAA) developed the PBOR in 1977 and revised it in 2017. The PBOR is designed so that you can know what to expect and what is reasonable for you to ask for when you receive care. If you haven’t already looked over the PBOR, please take time to familiarize yourself. In addition, if you use ostomy or urological supplies, here is what you should understand and expect when receiving medical care in your home.
Be Prepared
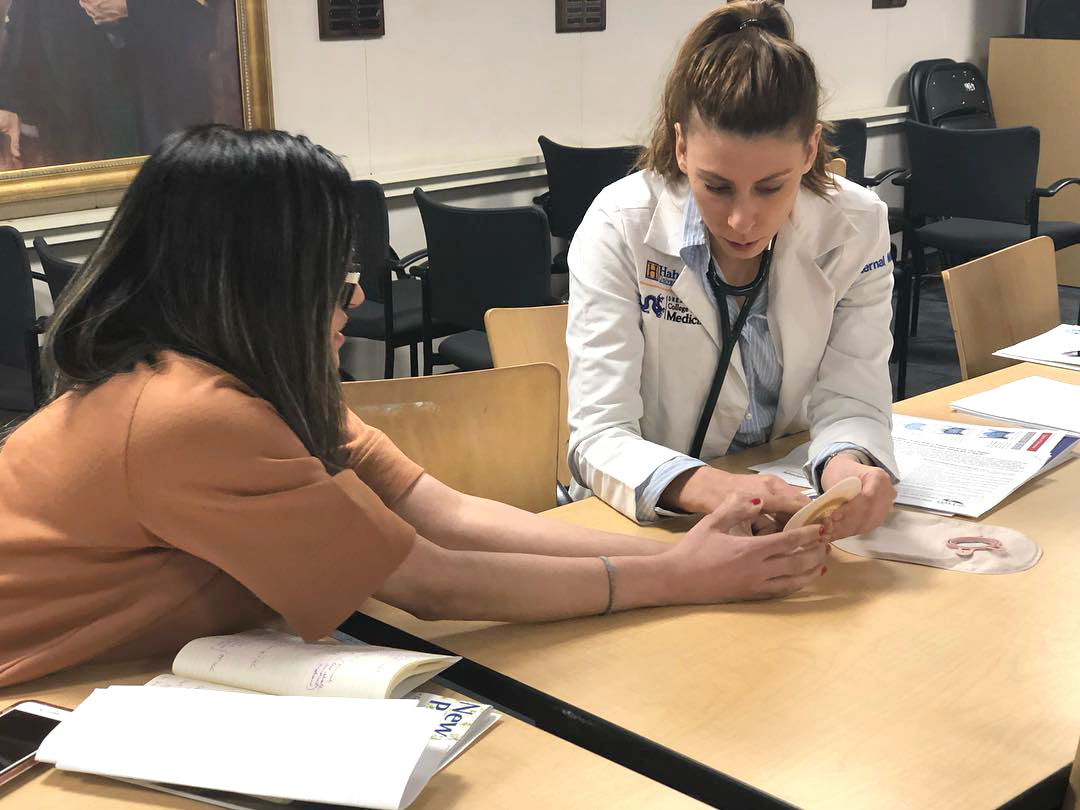
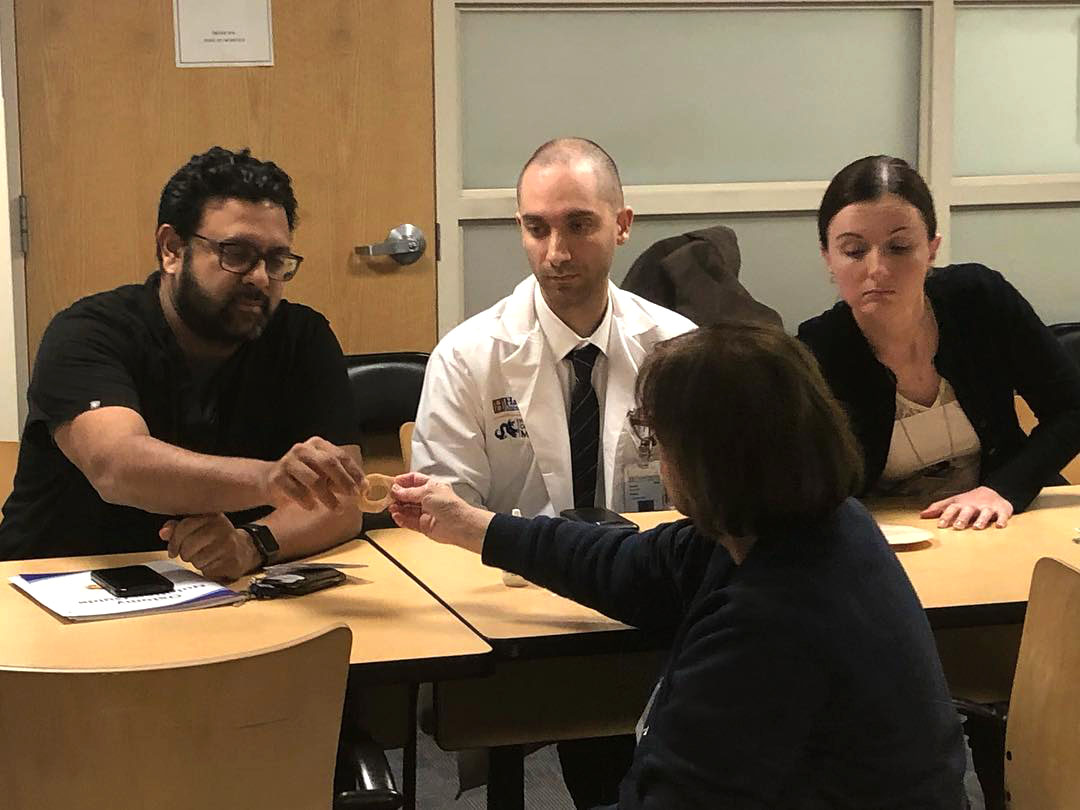
Be prepared in advance to take appropriate steps to ensure you receive quality ostomy care. As you prepare for discharge to home after your ostomy surgery, ask your case manager to make sure your home health agency has a certified ostomy nurse. This will also be important if you are a person already living with an ostomy with a new medical condition (such as hip surgery or a stroke). Your home health nurse should re-evaluate your ostomy care. For example, someone with arthritis may have lost dexterity and now needs to switch to a different type of pouching application system or you may have gained or lost some weight over the hospitalization (which can change your abdominal contours and your stoma) and now your current system doesn’t give you 2-5 days wear time anymore.
Change Agencies if Needed
If you are already home and your home health agency does not have a certified ostomy nurse, then request that they consult with one to ensure that you receive the proper optimal care. I often get phone calls or emails from colleagues who work for other agencies asking me ostomy questions or asking if I can come to see their patient. We are all in this together and we all want what is best for the patient, which is YOU! Don’t be afraid to ask for an ostomy nurse!
You may even have to change agencies. It isn’t difficult even though your current agency will likely not want you to change. You have a right to explain that you must receive your care from a certified ostomy nurse and your current agency, unfortunately, does not provide this type of care. All you have to do is call the agency YOU choose and tell them you want to transfer your care to their agency. Typically the new agency will contact your doctor or ask you to let your doctor know you want to change agencies. The new agency will then inform your current home health agency that they are taking over your care.
What to do if an Ostomy Nurse is Still Not Available?
If all else fails and for whatever reason you have a home health agency without access to a certified ostomy nurse, you still have resources. You can:
- Go to www.wocn.org and look up a patient referral for an ostomy nurse in your area. This content also usually includes contact information for the WOC Nurse in your area.
- Visit www.ostomy.org for educational resources such as the New Ostomy Patient Guide and UOAA has a dedicated webpage specifically for Ostomy Health Care Resources.
- Use social media to find others that may be in the same situation as you. There are a multitude of Facebook pages/groups for ostomates with WOC nurses who follow these groups and offer comments or suggestions when specifically asked.
In Conclusion
We cannot say this enough: YOU have a right to quality care and deserve quality care. Know your rights. You deserve to be able to live your life to the fullest with your new or established ostomy.
Patients and medical professionals can work together to improve patient outcomes. If you want to help UOAA drive change and achieve ostomy quality of care improvements for patients while under home care, please print and share these resources with your home health agency: Achieve 5 Star Ostomy Home Health Care and Important Reminders for Home Health Providers Treating People with an Ostomy.